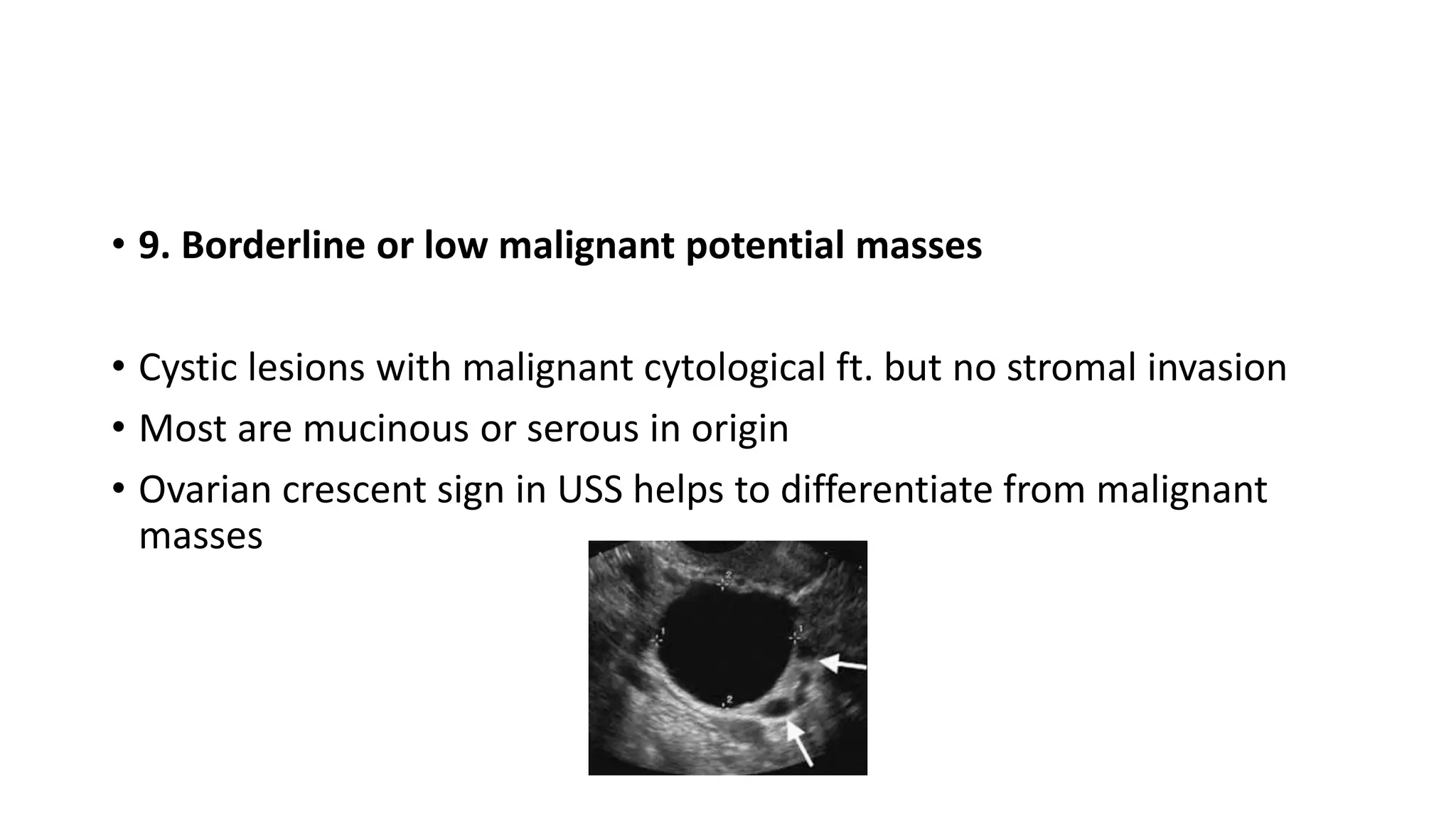
This document discusses the management of adnexal masses in pregnancy. It notes that adnexal masses occur in 0.1-8.8% of pregnancies, with ovarian malignancy found in 1 in 1500-32000 pregnancies. Most masses are benign and can be managed conservatively. Clinically significant masses include corpus luteum cysts, follicular cysts, hemorrhagic cysts, ovarian hyperstimulation syndrome, and dermoid cysts. Assessment involves ultrasound and tumor markers. Conservative management is recommended for most simple cysts under 5cm. Larger or complex cysts should be monitored. Surgery, including possible laparoscopy, is indicated for adnexal torsion, suspected malignancy