- The risk of retinal tear (RT) or retinal detachment (RRD) associated with acute posterior vitreous detachment (PVD) seen in a comprehensive eye care setting is lower than rates reported in retina specialty clinics.
- Several factors can help predict complications, including blurred vision, age younger than 60, prior eye surgery, symptoms less than 1 week, family retinal detachment history, floaters, flashes, vitreous pigment, hemorrhage, lattice degeneration, and vision worse than 20/40.
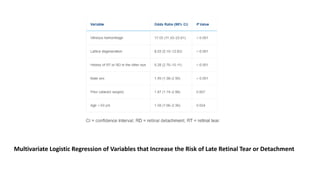
- High-risk factors for late complications included vitreous hemorrhage, lattice degeneration, or history of RT or RRD in the fellow eye. Close follow-