1. Acute otitis media (AOM) is a pyogenic infection of the middle ear cleft lasting less than 3 weeks, which can occur via the Eustachian tube, tympanic membrane perforation, or hematogenous spread. Common causes include respiratory infections and exposure to cigarette smoke.
2. Otitis media with effusion is the presence of middle ear fluid without signs of infection. It is common in young children and can be caused by poor Eustachian tube function or follow AOM.
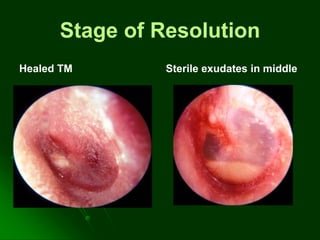
3. Treatment for AOM includes antibiotics, nasal decongestants, and analgesics while treatment for persistent or recurrent OME may include antibiotics, steroids, myringotomy