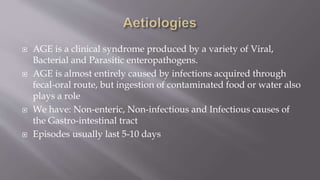
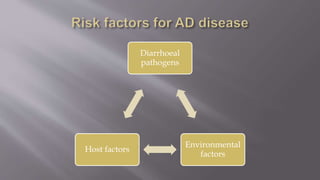
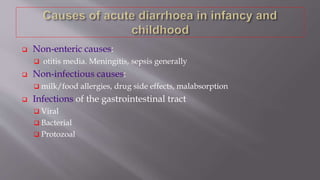
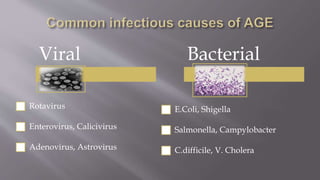
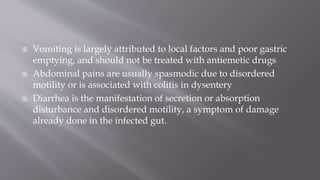
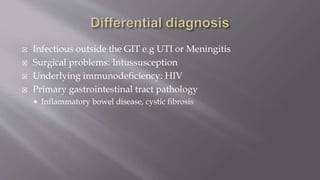
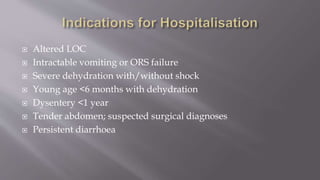
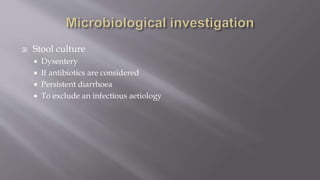
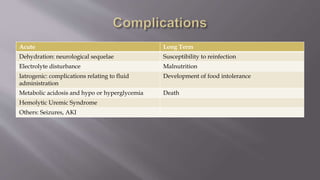
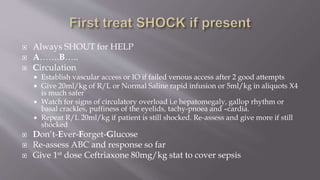
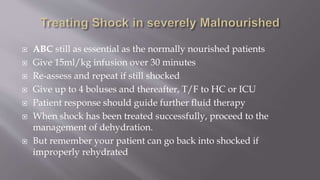
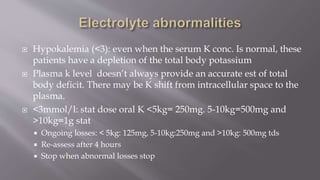
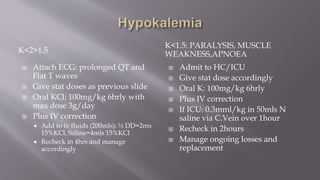
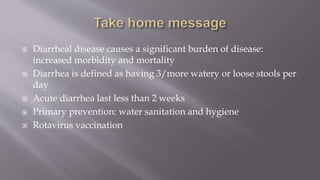
This document provides an overview of acute diarrhea in children, including definitions, epidemiology, causes, pathophysiology, signs and symptoms, complications, diagnosis, and management. It discusses the major infectious causes of diarrhea like rotavirus. It outlines the approach to assessing dehydration and managing rehydration. Complications are addressed. Differential diagnosis and management of specific cases like dysentery are also covered. Nutritional support and prevention strategies are highlighted. Key references on the topic are provided.