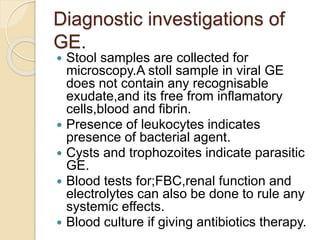
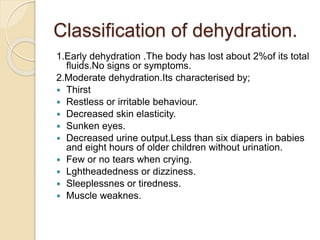
This document provides an overview of gastroenteritis in pediatrics. It defines gastroenteritis as an inflammatory disease of the stomach and intestines characterized by sudden onset of diarrhea and/or vomiting. Common causes are viruses, bacteria, protozoa, and non-infectious agents. Symptoms and management depend on the cause. Treatment involves rehydration and replacement of fluids and electrolytes to prevent dehydration, along with any necessary medical treatment of the underlying infection. Nutritional management is also important during treatment and recovery.