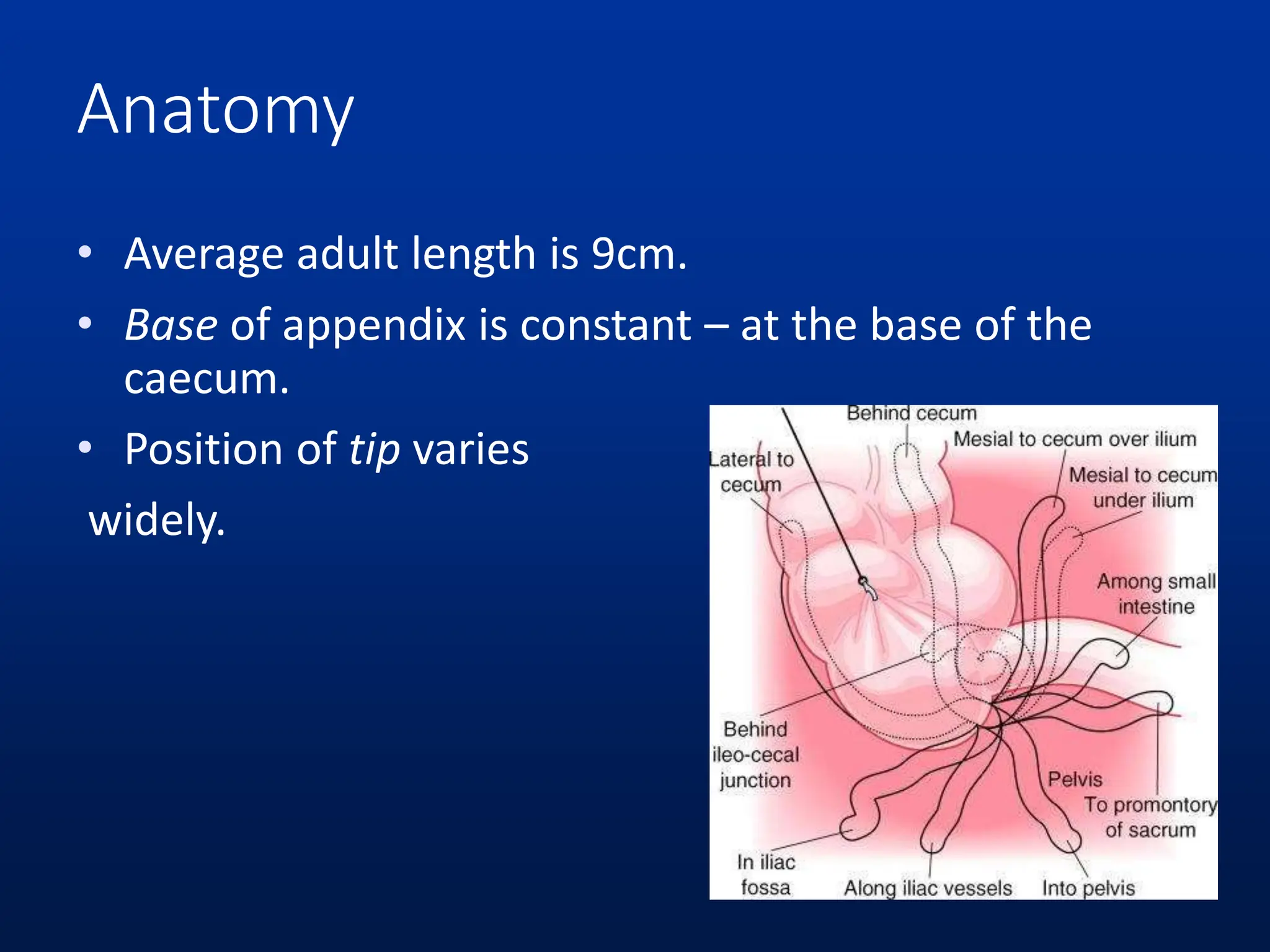
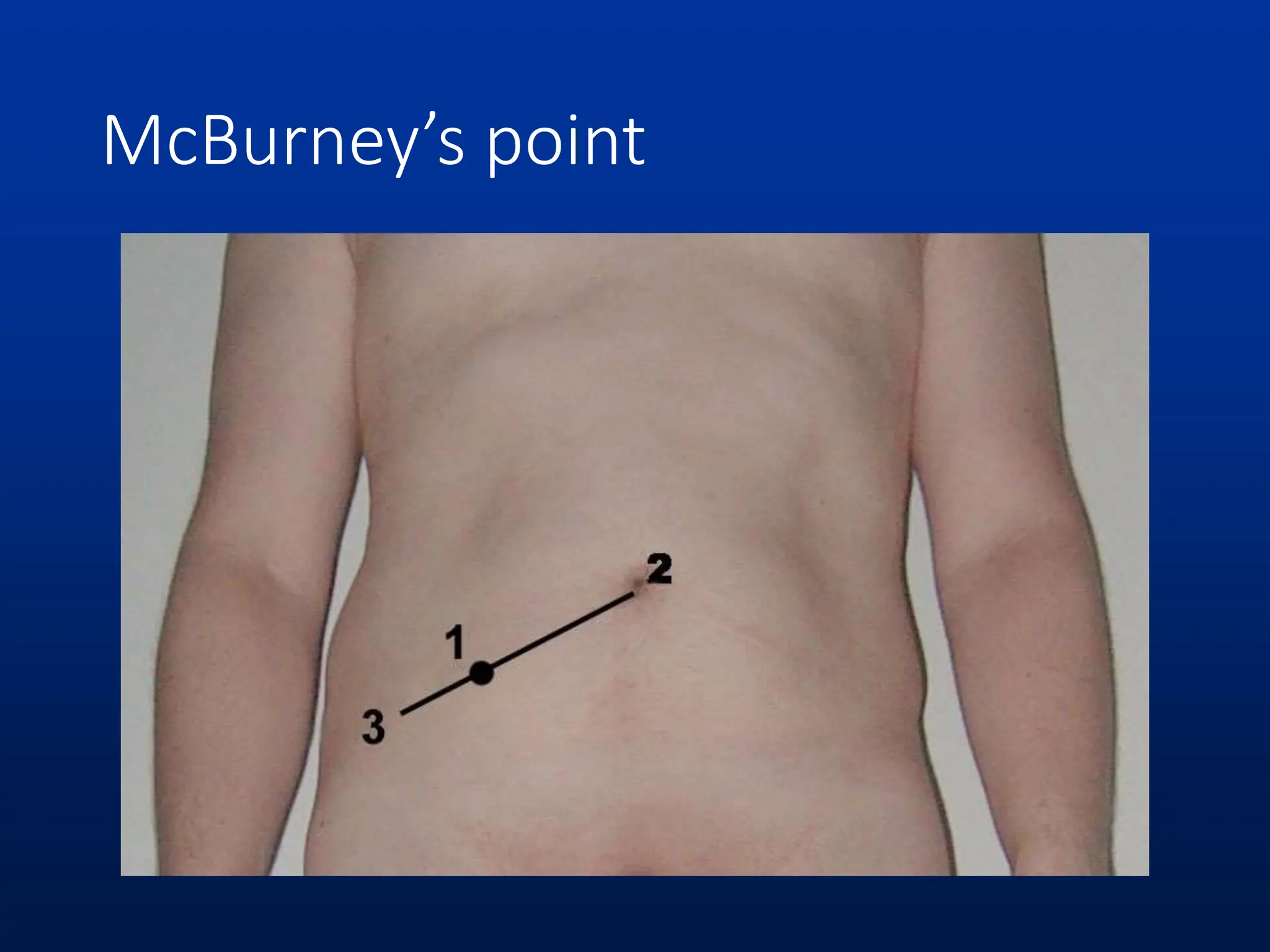
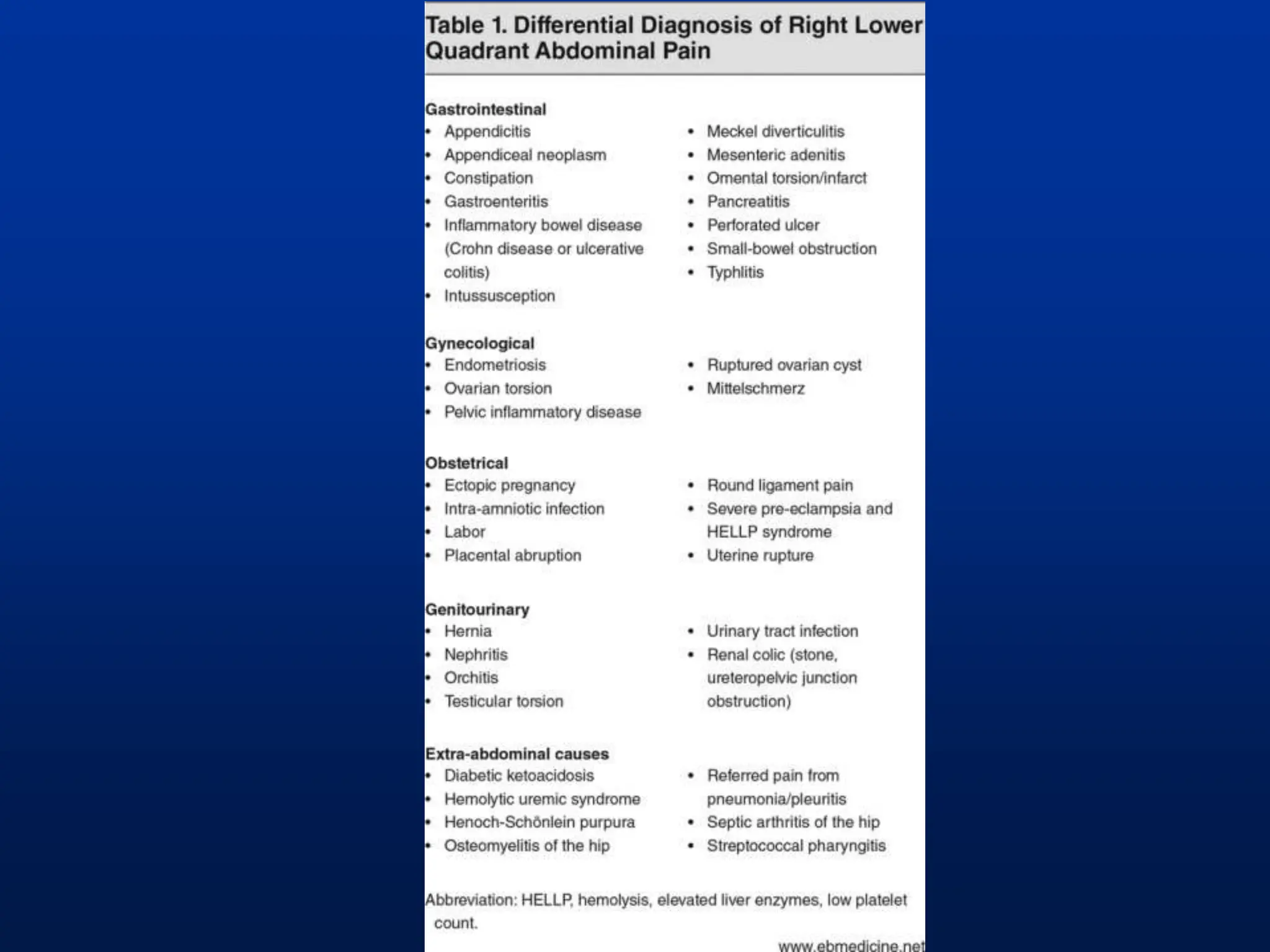
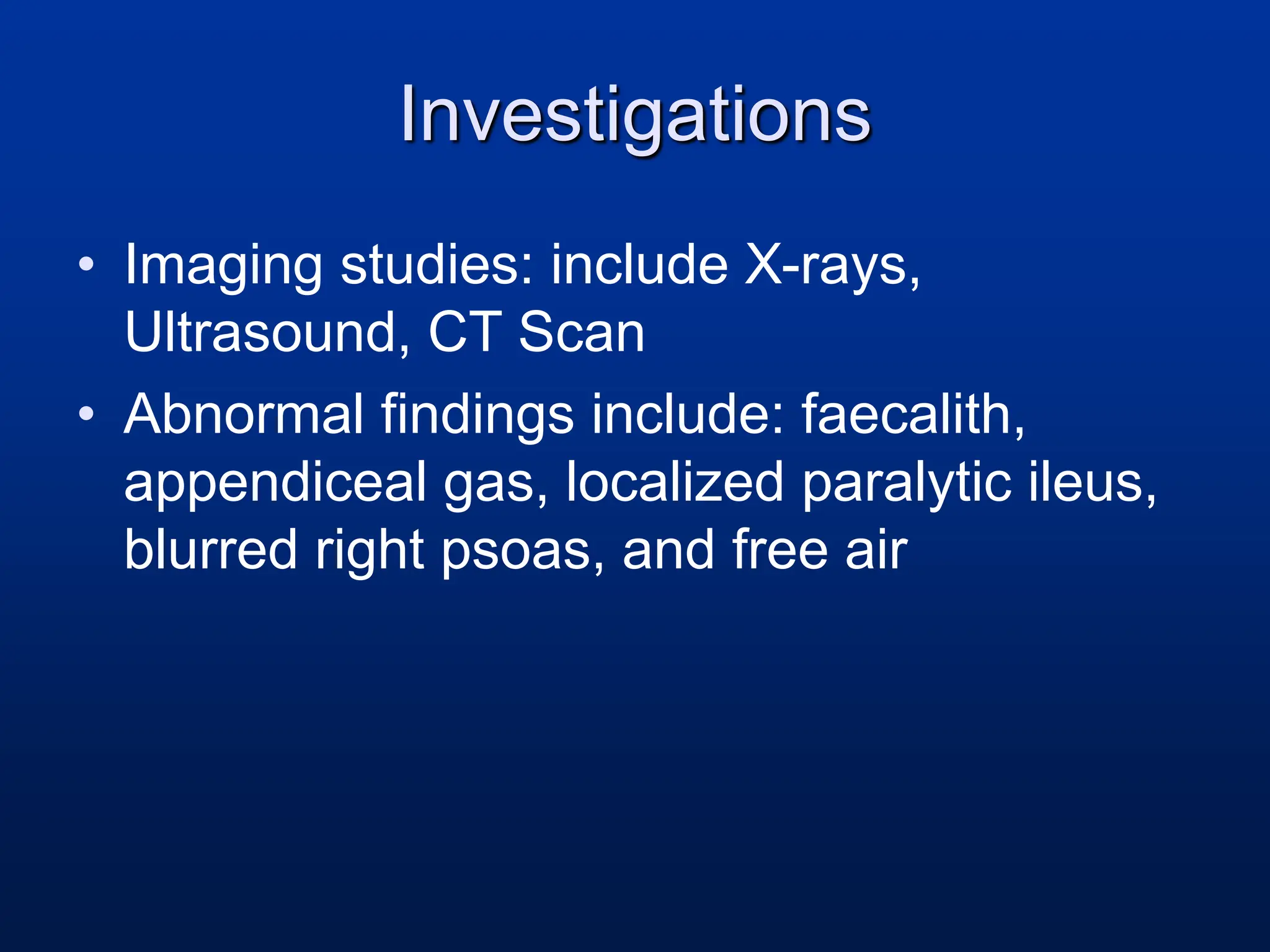
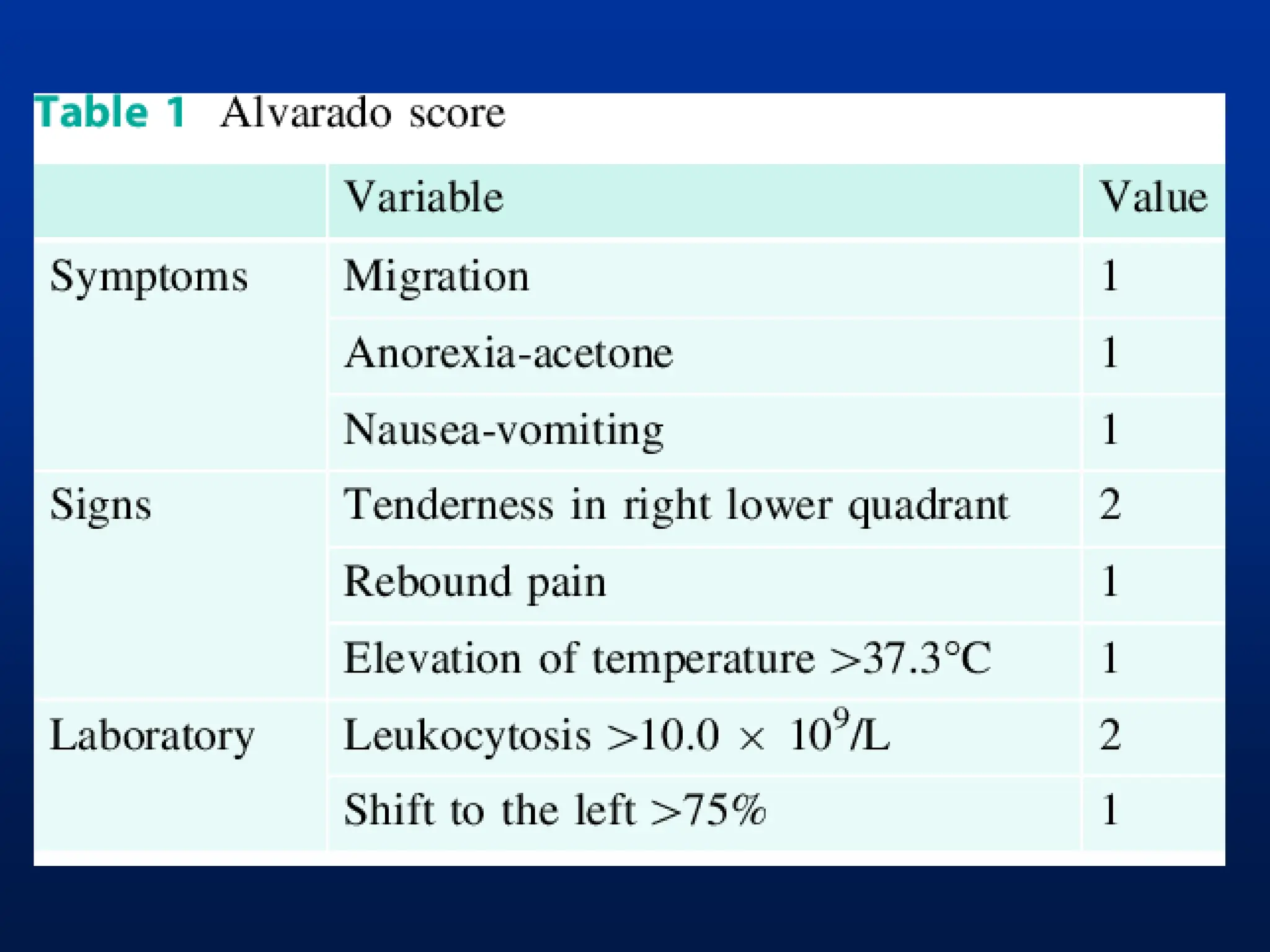
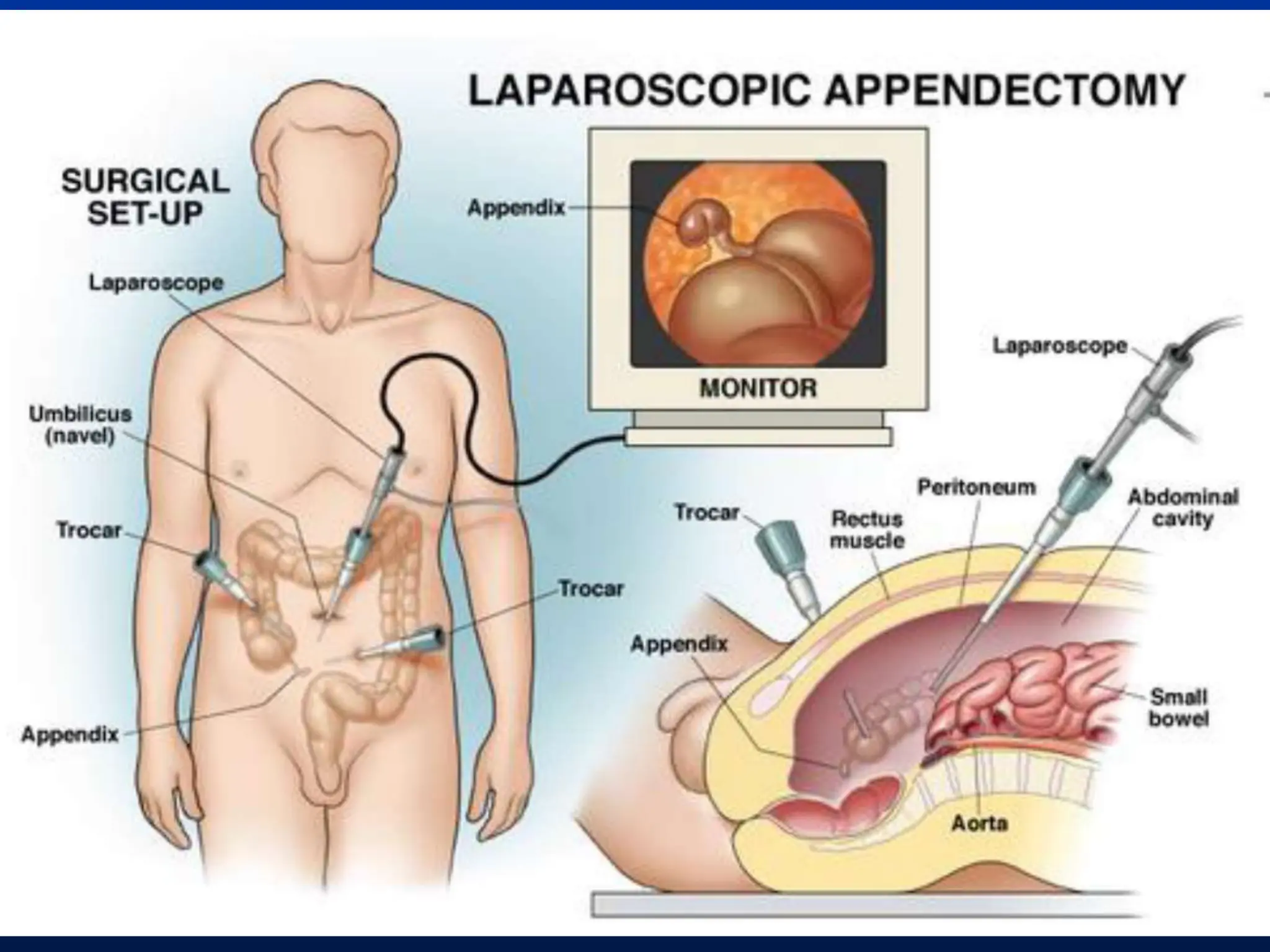
This document provides a comprehensive overview of appendicitis and appendicectomy, detailing the anatomy, etiology, symptoms, and physical examination findings associated with acute appendicitis. It emphasizes the treatment protocol of appendicectomy, which can be performed via laparotomy or laparoscopy, and outlines the necessary nursing responsibilities and post-operative care. Additionally, the document addresses complications, special populations, and investigative measures essential for accurate diagnosis.