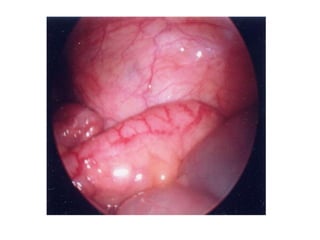
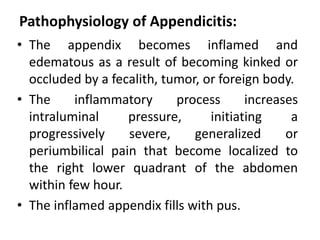
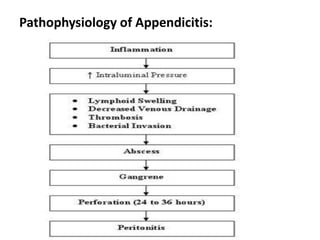
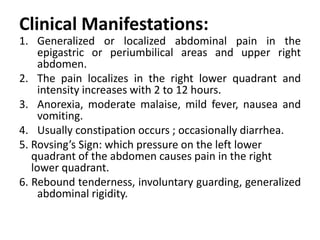
Appendicitis is the inflammation of the appendix, most commonly affecting individuals aged 10-30, particularly males, and is often caused by obstruction leading to infection. Symptoms include abdominal pain that localizes to the right lower quadrant, nausea, and fever, with diagnosis supported by physical examination and imaging tests. Treatment typically involves an appendectomy, along with intravenous fluids and antibiotics to manage the condition and prevent complications.