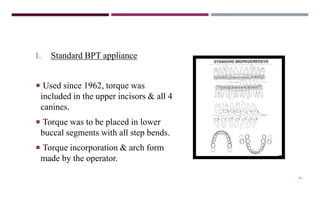
Bioprogressive Therapy (BPT) is a fixed orthodontic technique developed by Dr. Robert Murray Ricketts that focuses on comprehensive facial treatment rather than just teeth alignment. It emphasizes biological progressions in growth and function and utilizes specific principles, such as torque control, muscular anchorage, and visual treatment objectives to optimize treatment outcomes. The therapy incorporates a management system to ensure quality, quantity, and effectiveness in orthodontic care.