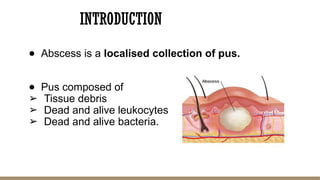
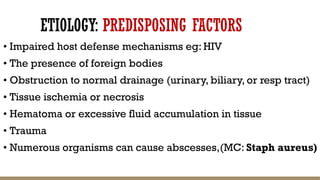
An abscess is a localized collection of pus caused by various factors, including infections, trauma, and iatrogenic causes. Symptoms include fever, pain, and signs of inflammation, while complications can lead to severe health issues like organ dysfunction and bacteremia. Diagnosis involves laboratory tests and imaging studies, with treatment options ranging from drainage and antibiotics to conservative management.