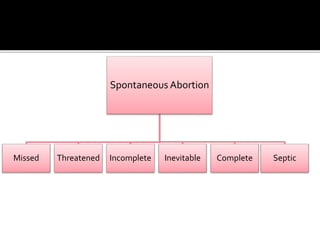
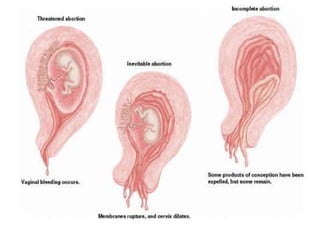
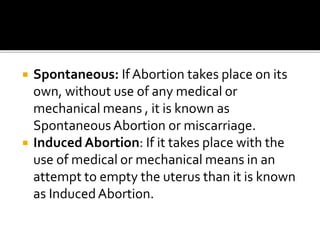
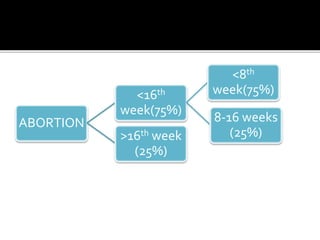
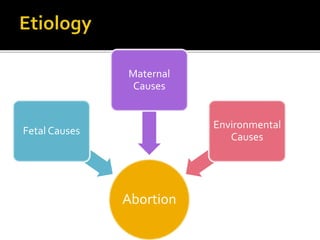
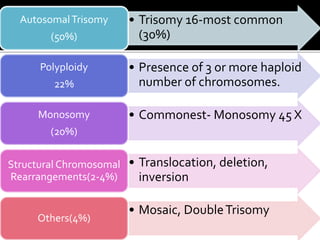
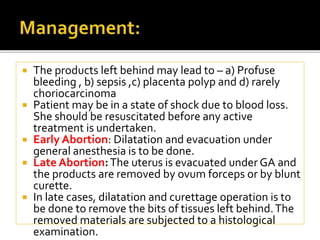
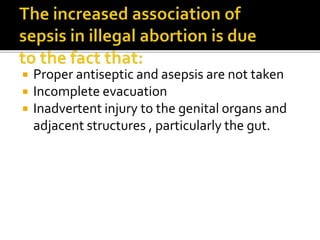
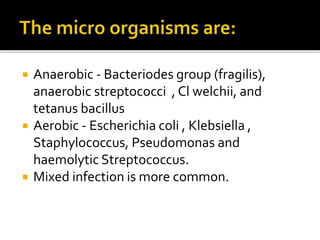
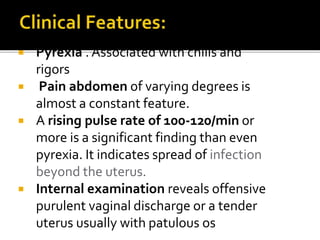
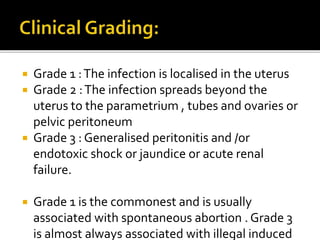
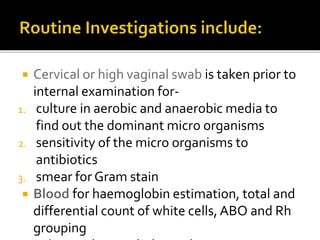
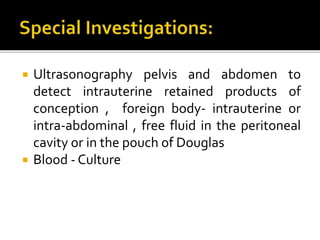
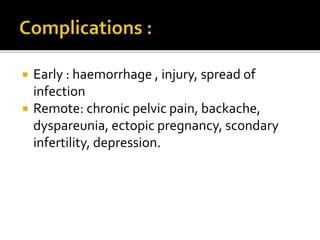
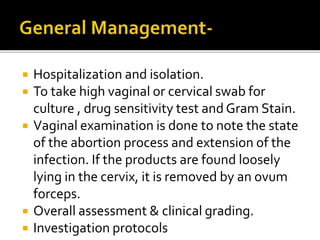
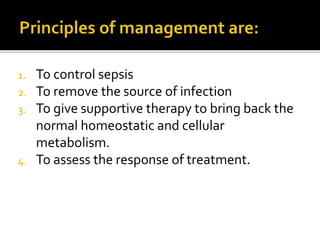
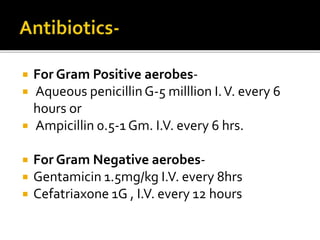
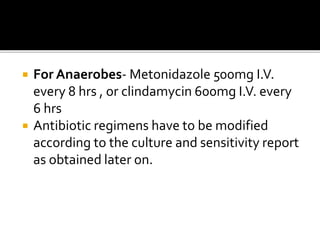
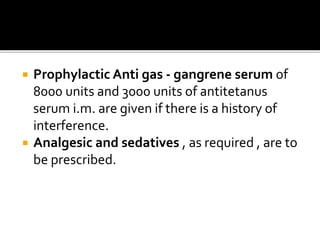
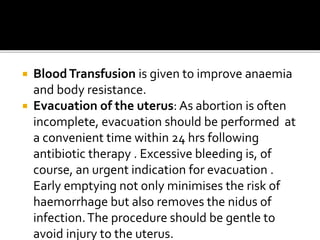
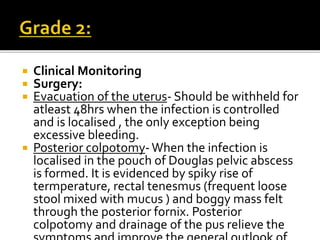
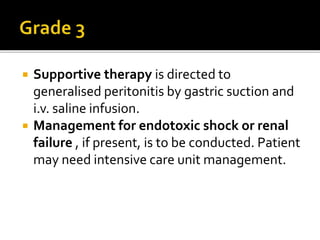
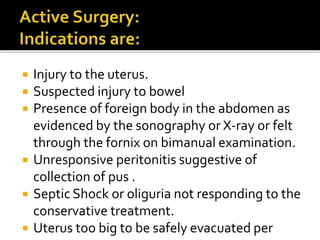
The document discusses the various aspects of abortion, including definitions, types (spontaneous and induced), causes related to fetal, maternal, and environmental factors, and the clinical management of complications. It details diagnostic methods, treatments for different types of abortion, and the implications of emergency situations such as septic abortion while emphasizing the importance of careful monitoring and management. Additionally, it addresses recurrent miscarriage and possible treatments like progesterone supplementation and low dose aspirin.