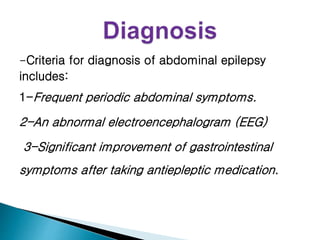
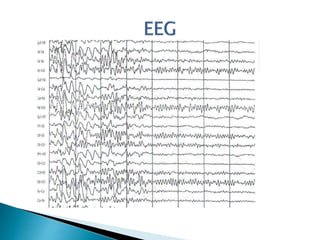
Abdominal epilepsy is a rare condition characterized by gastrointestinal disturbances caused by epileptiform seizure activity in the brain. It can present with abdominal pain, vomiting, and lethargy. Diagnosis involves recurrent abdominal symptoms, abnormal EEG findings, and improvement of gastrointestinal symptoms with antiepileptic medication. A case study describes an 18-year-old female patient who presented with recurrent abdominal pain and was diagnosed with abdominal epilepsy based on normal test results but abnormal EEG findings showing seizure activity. She responded well to treatment with topiramate.