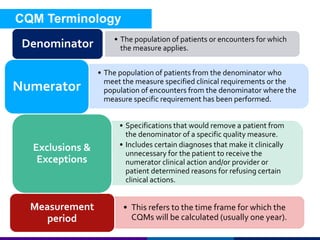
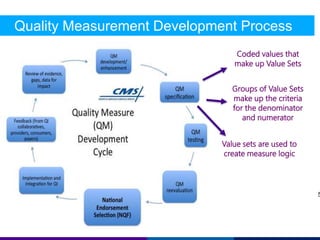
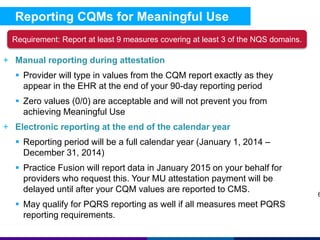
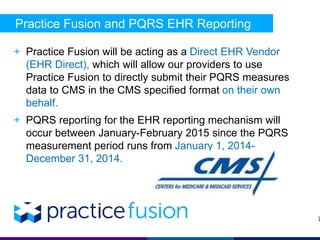
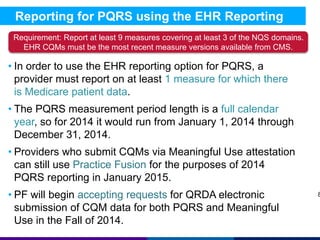
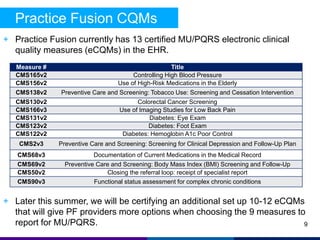
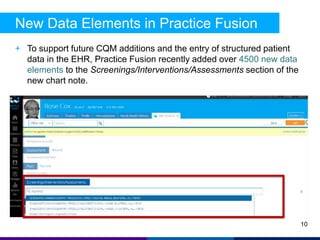
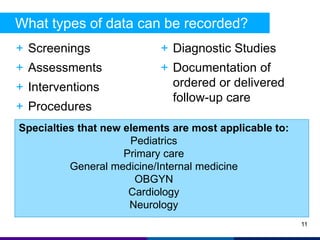
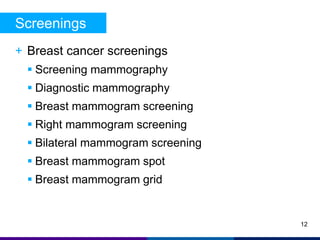
The document provides an overview of clinical quality measure (CQM) reporting in Practice Fusion, detailing its significance in measuring healthcare quality and outcomes. It outlines the processes for both manual and electronic reporting of CQMs for meaningful use and PQRS, including requirements for measure selection and reporting timelines. Additionally, it highlights new data elements added to the platform to enhance quality reporting and patient care.