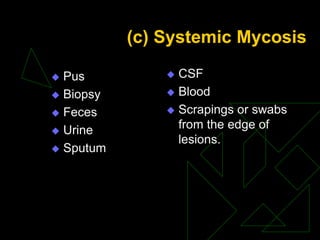
This document discusses the laboratory diagnosis of fungal infections through microscopic, cultural, and serological methods. It outlines how to collect and transport clinical specimens depending on the type of suspected fungal infection (superficial, subcutaneous, or systemic). Direct microscopic examination techniques include wet mounts, stains, and histopathology. Fungal cultures are grown on general and selective media and identified based on morphology and biochemical assays. Serological tests detect antigens or antibodies. Together, these laboratory methods allow identification of the infecting fungus.