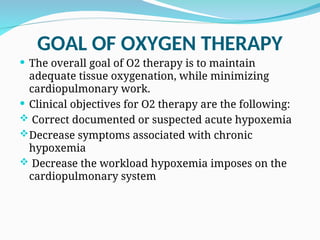
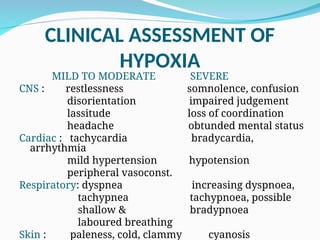
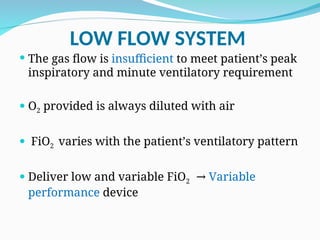
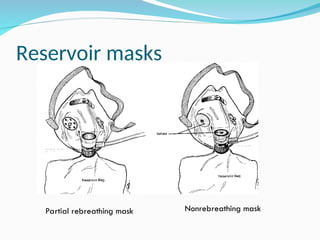
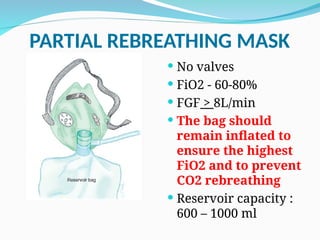
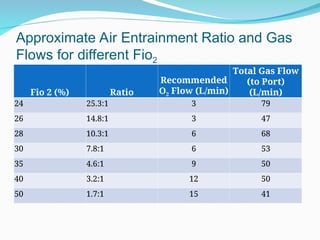
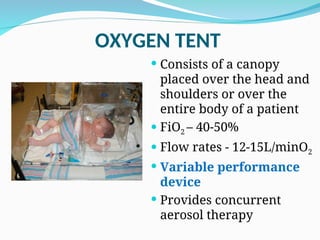
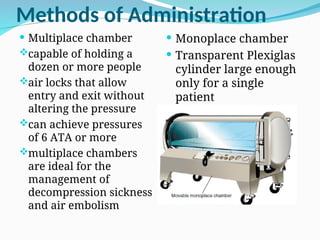
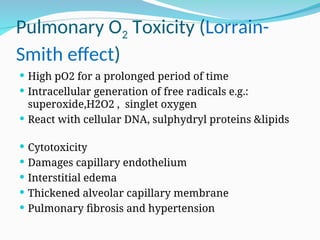
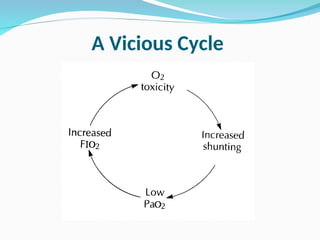
The document outlines the objectives and goals of oxygen therapy (O2 therapy), emphasizing the need to maintain adequate tissue oxygenation while minimizing cardiopulmonary work. It describes various indications for O2 therapy, the classifications of delivery systems (low flow and high flow systems), their administration techniques, and associated complications such as oxygen toxicity and fire hazards. Additionally, the document details the clinical assessment of hypoxia and the methods of O2 delivery, including devices for specific patient populations like infants.