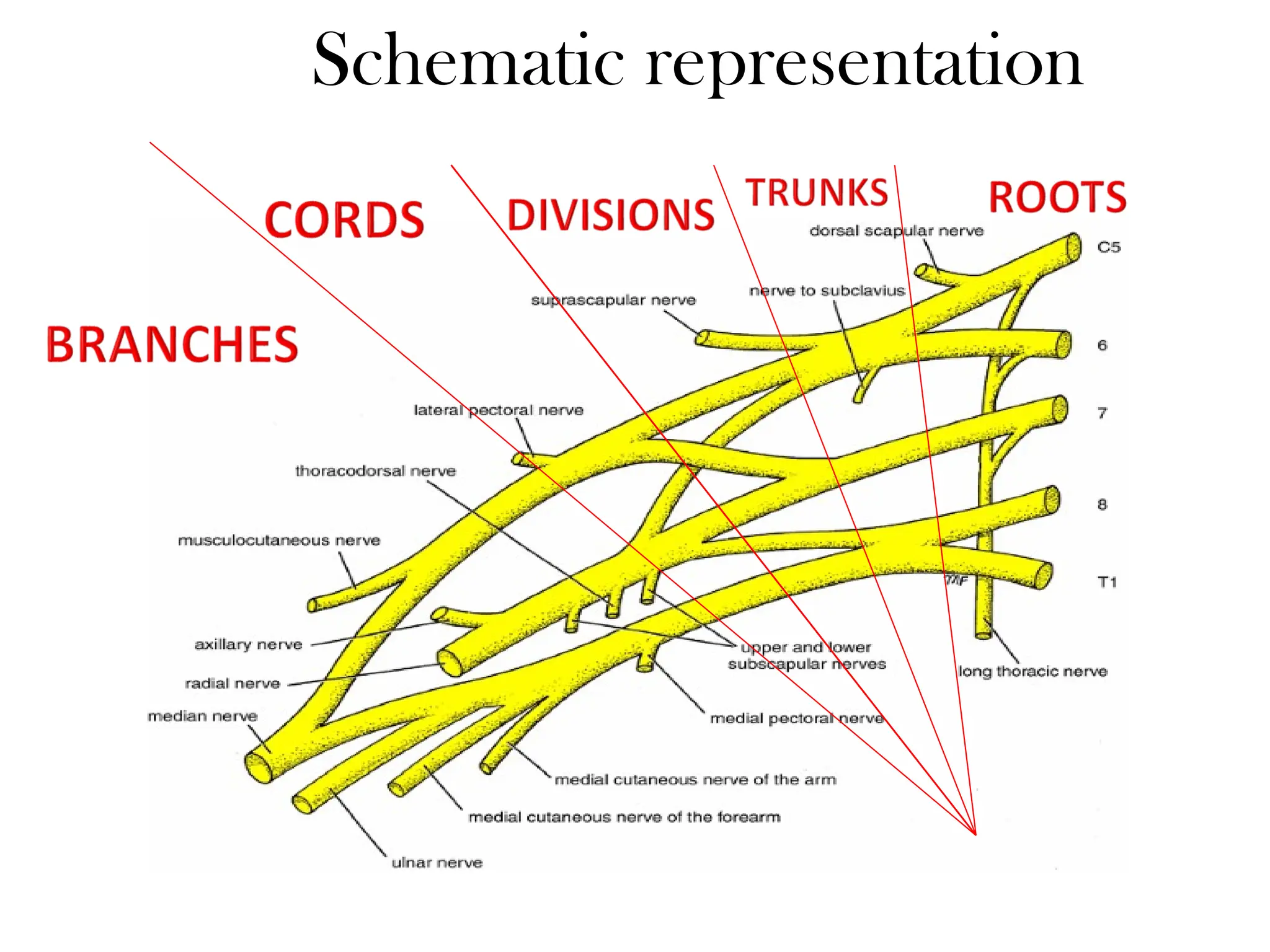
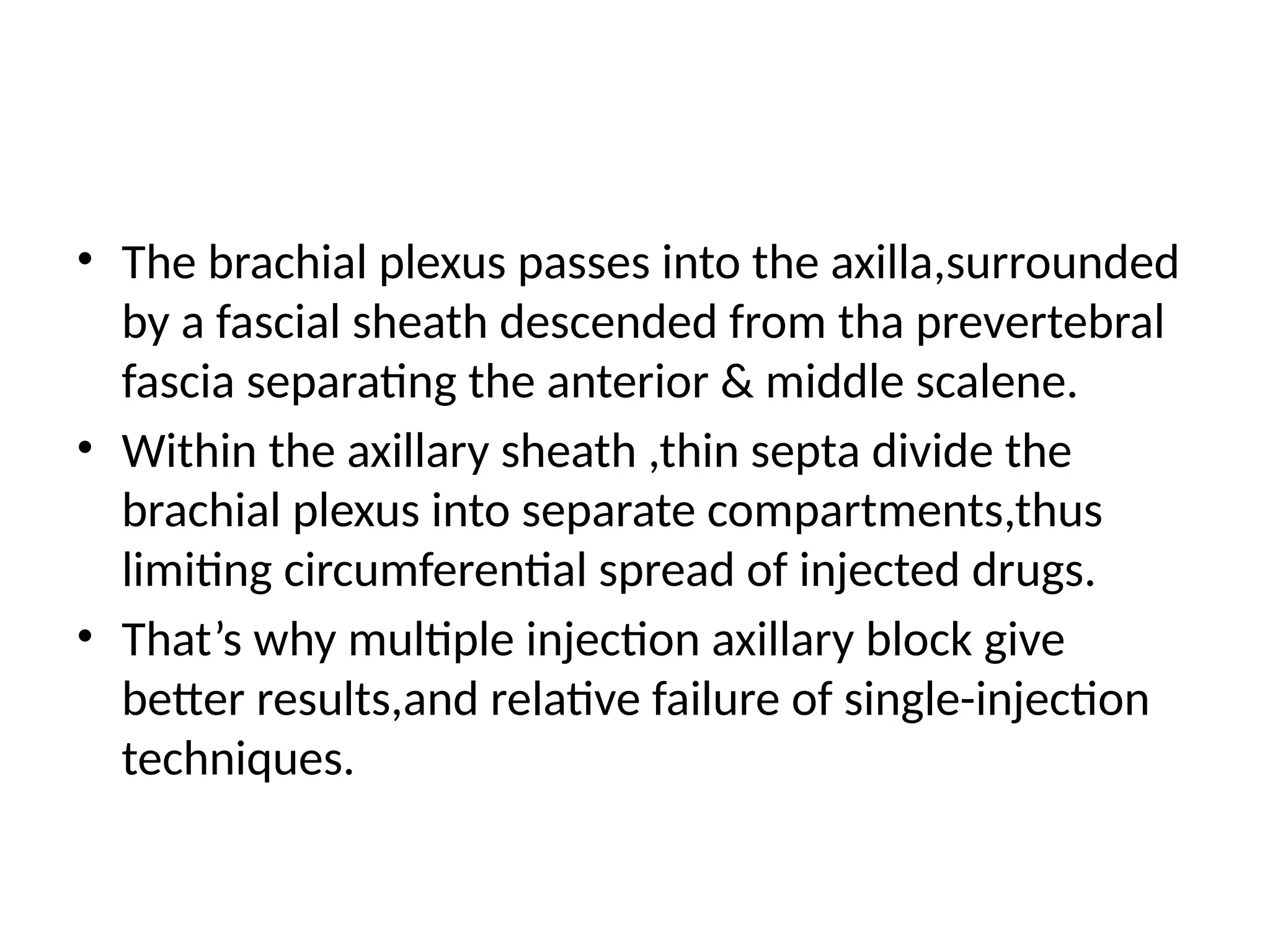
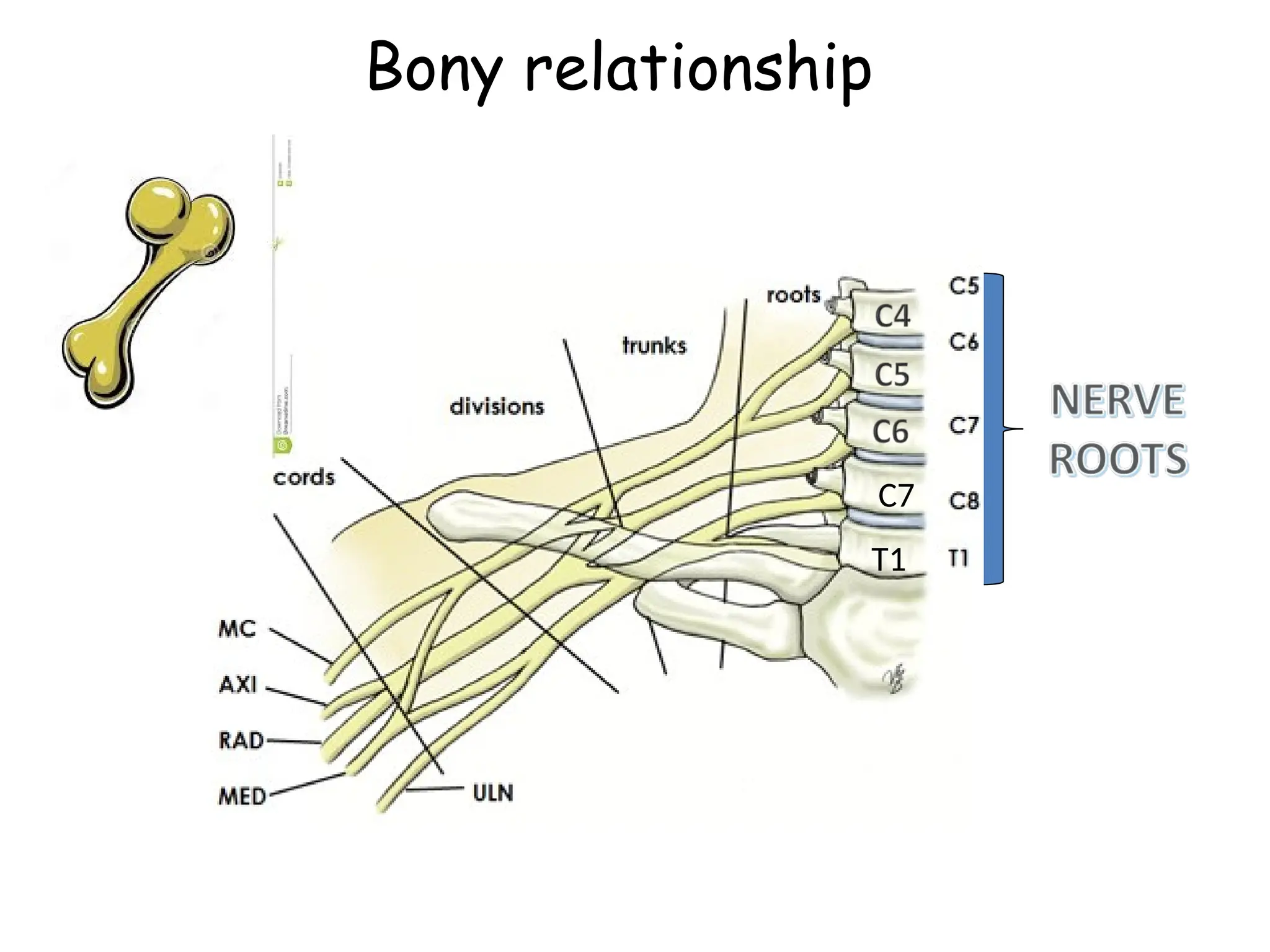
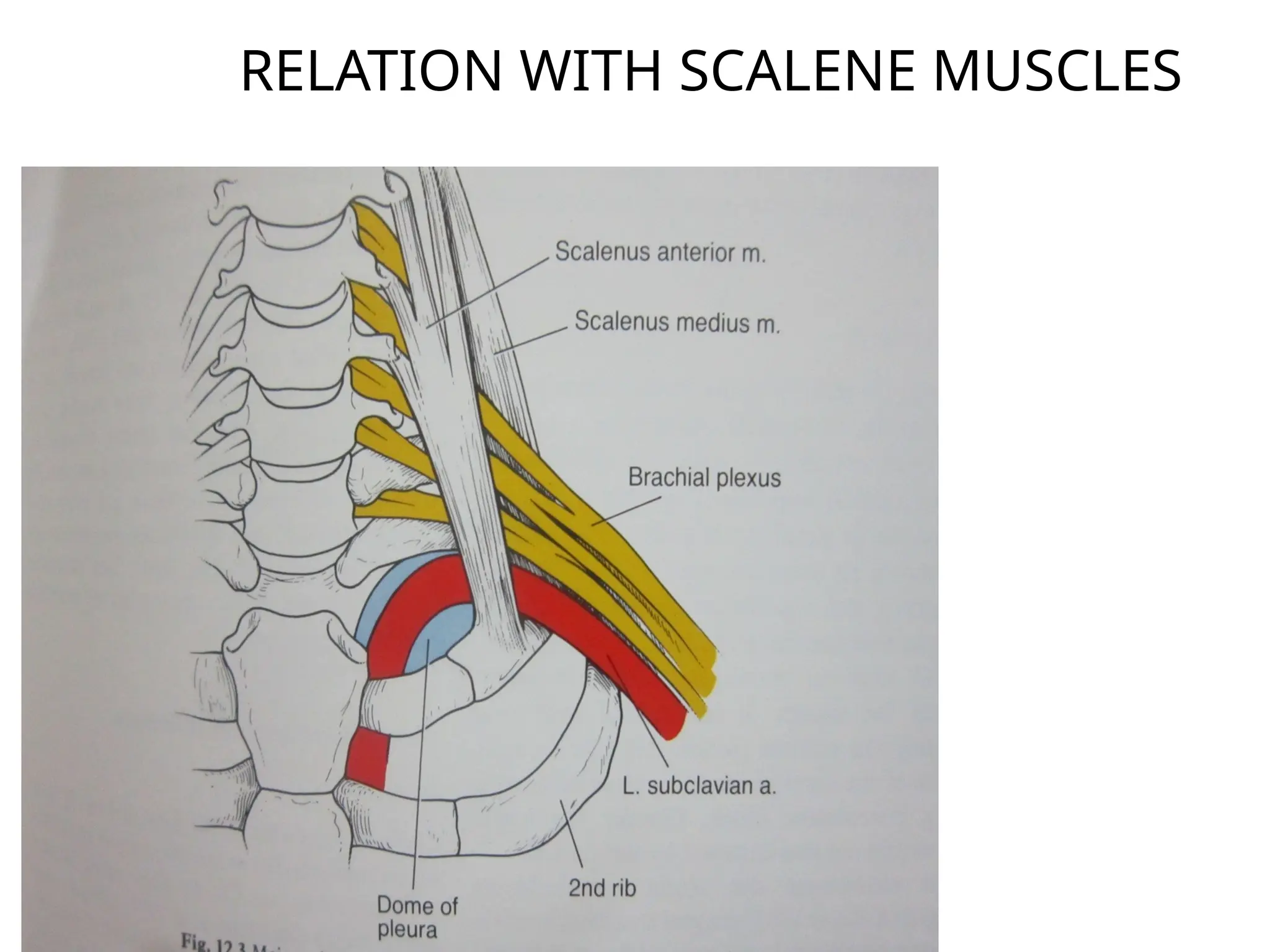
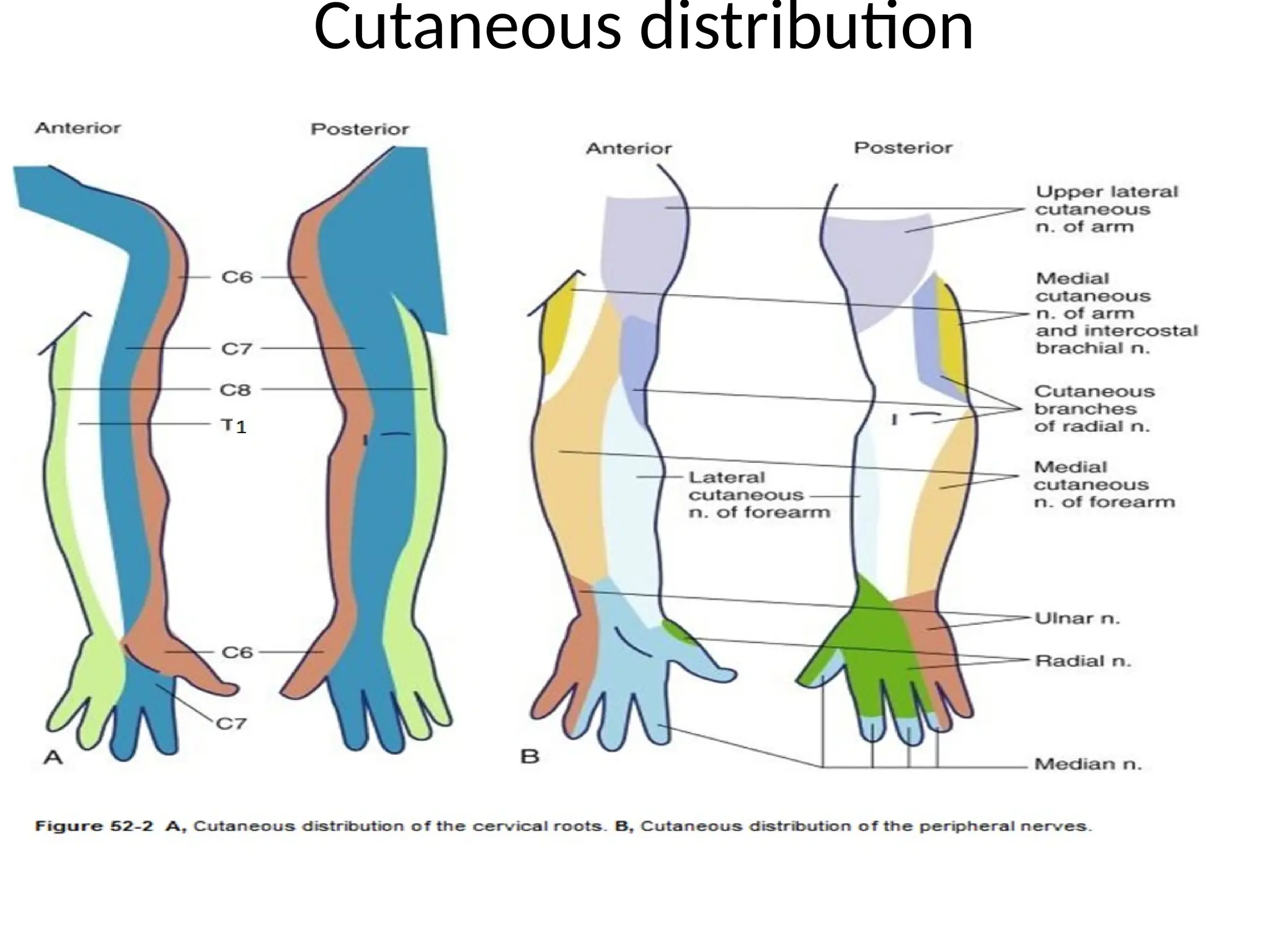
The document discusses the anatomy, technique, and clinical applications of the interscalene block for anesthesia during shoulder and upper arm surgeries. It describes the brachial plexus structure, various approaches for needle insertion, and assessment of sensory and motor blocks of nerves involved. Complications and contraindications of the procedure are also mentioned, emphasizing safe practice and effective pain management.