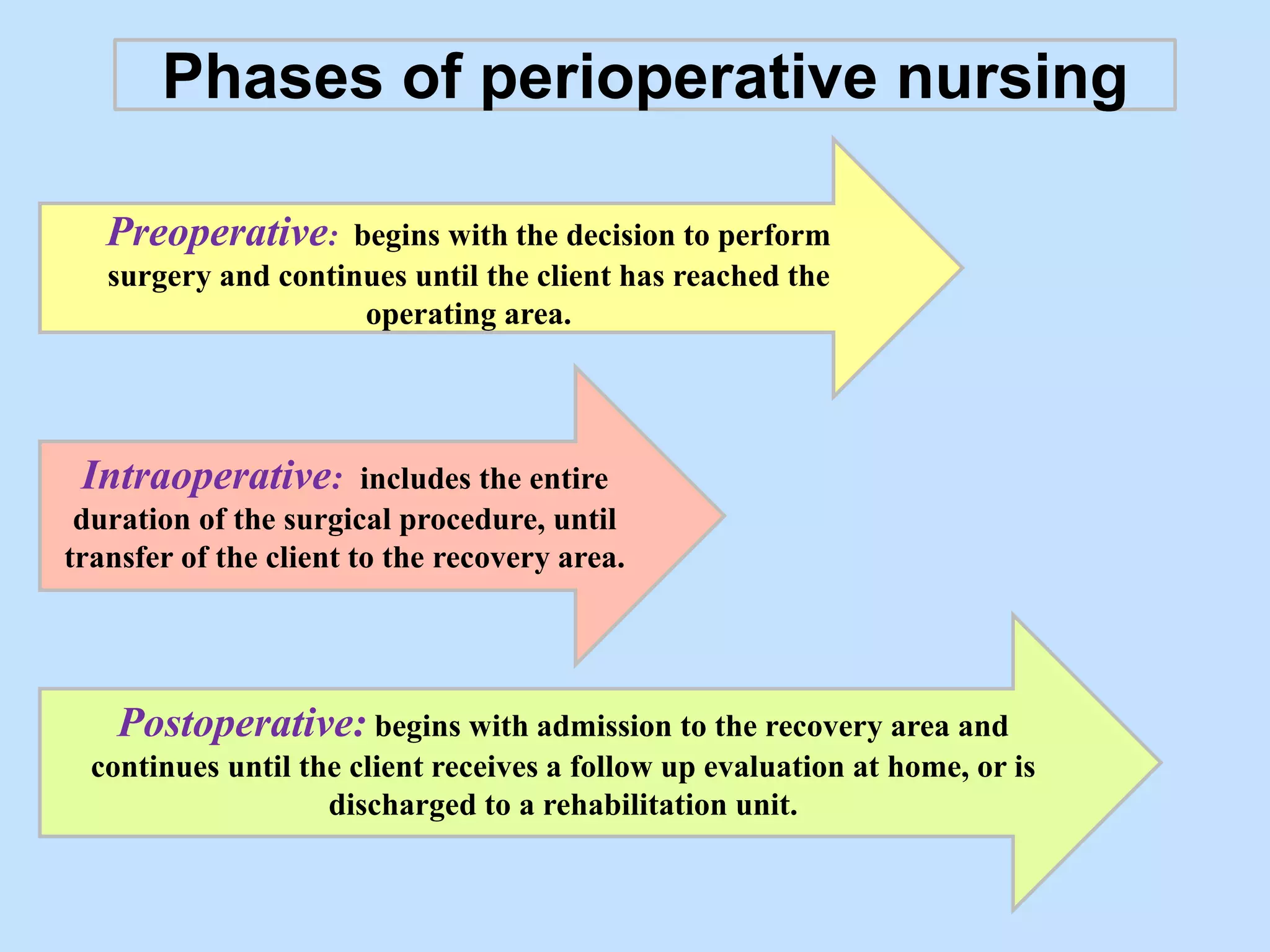
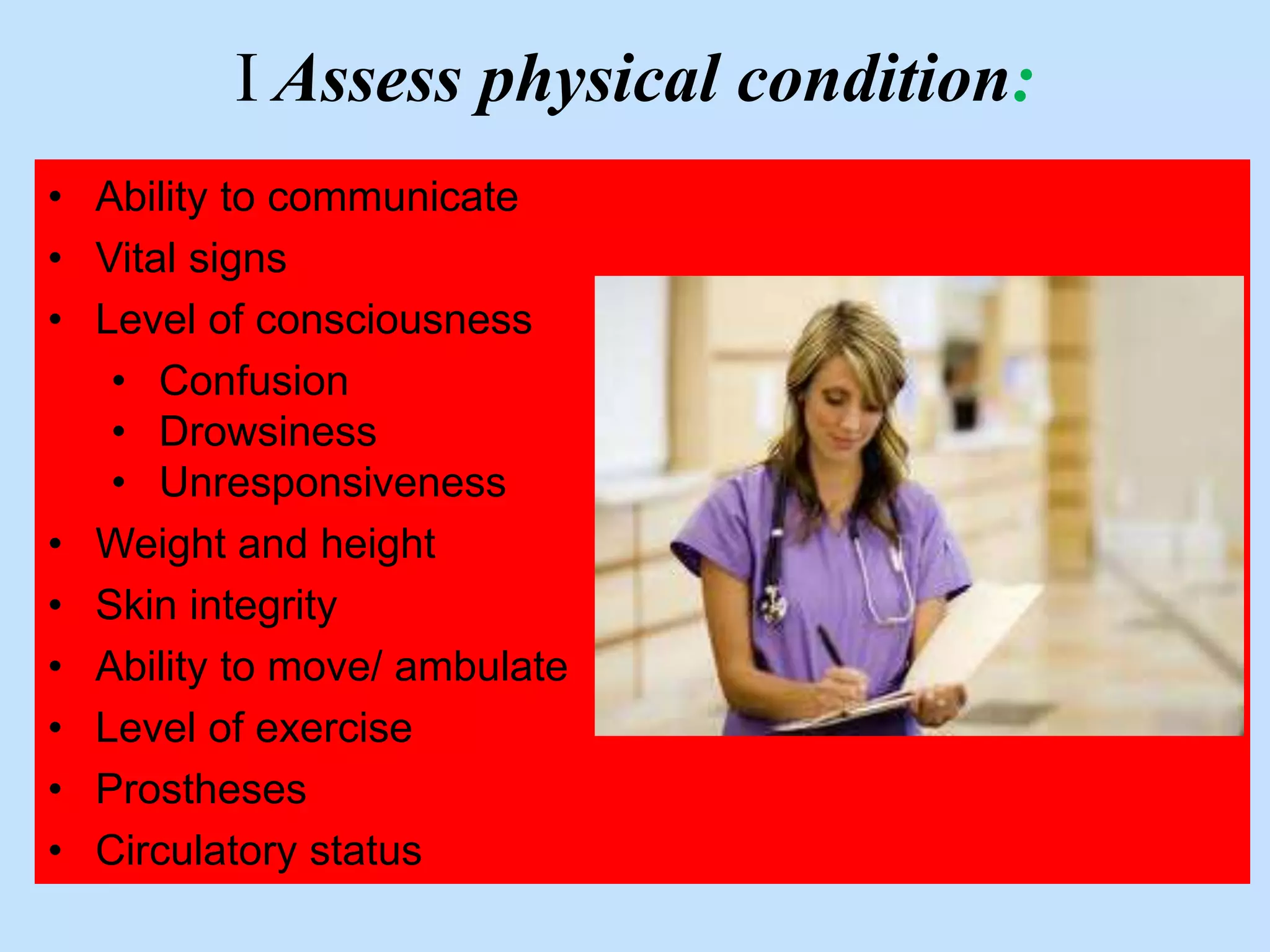
The document discusses the history and evolution of surgical nursing from the late 19th century to present day. It covers the development of specialized surgical nursing roles including circulating nurses, perioperative nurses, and advanced practice roles. The future of surgical nursing is discussed, highlighting trends toward increased specialization, advanced practice roles, and the need for skills in areas like informatics, technology management, and radiology to support more complex surgical procedures.