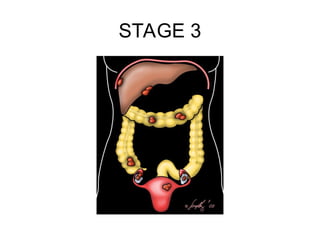
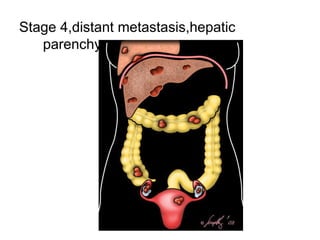
Ovarian cancer is a significant health concern, characterized by risk factors such as family history, genetic mutations (BRCA1/BRCA2), and personal health history. The prognosis heavily depends on tumor staging at diagnosis, with treatment options varying from surgery to chemotherapy based on disease operability. Accurate staging through imaging and surgical methods is crucial for effective management and improved patient outcomes.