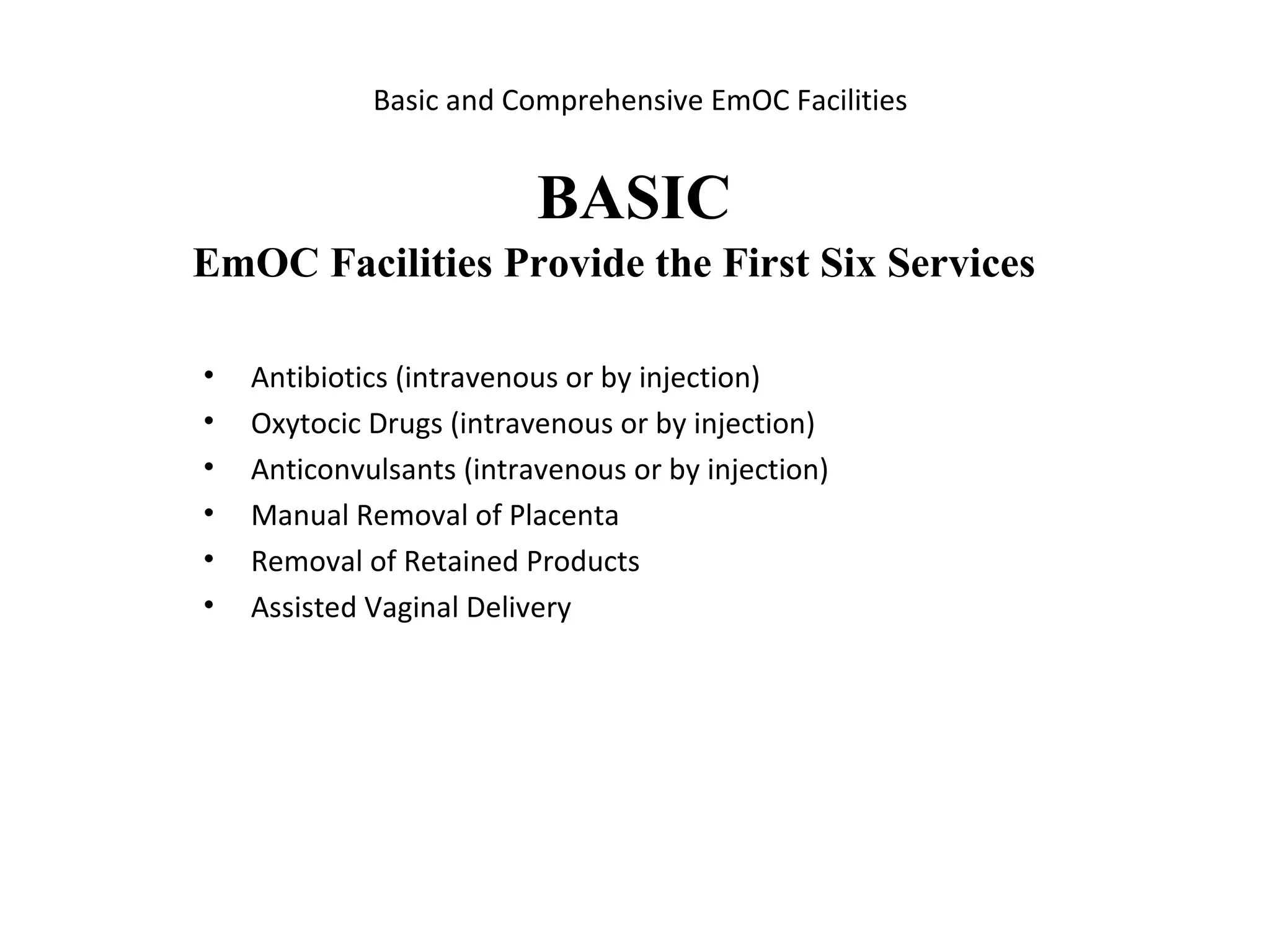
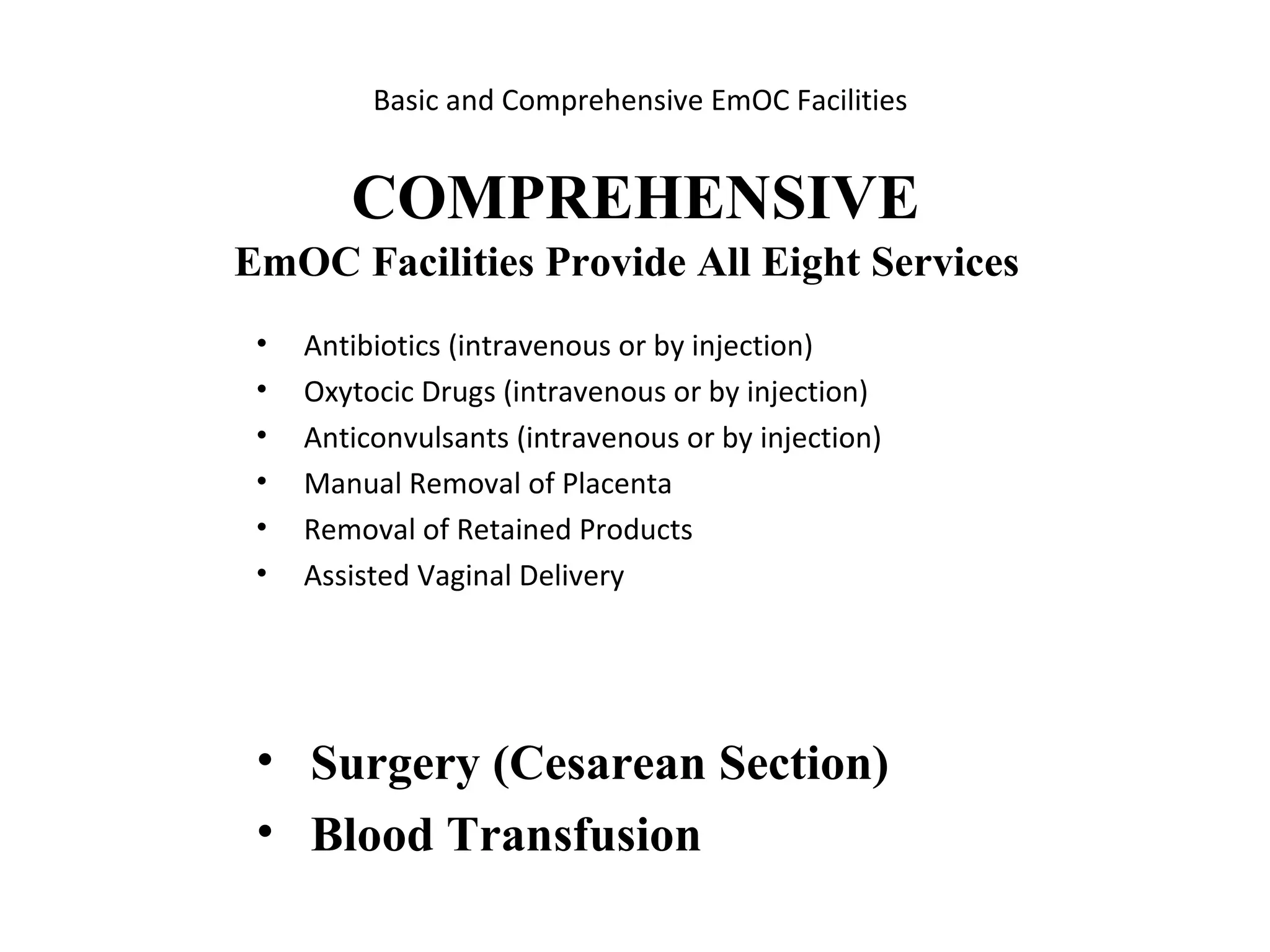
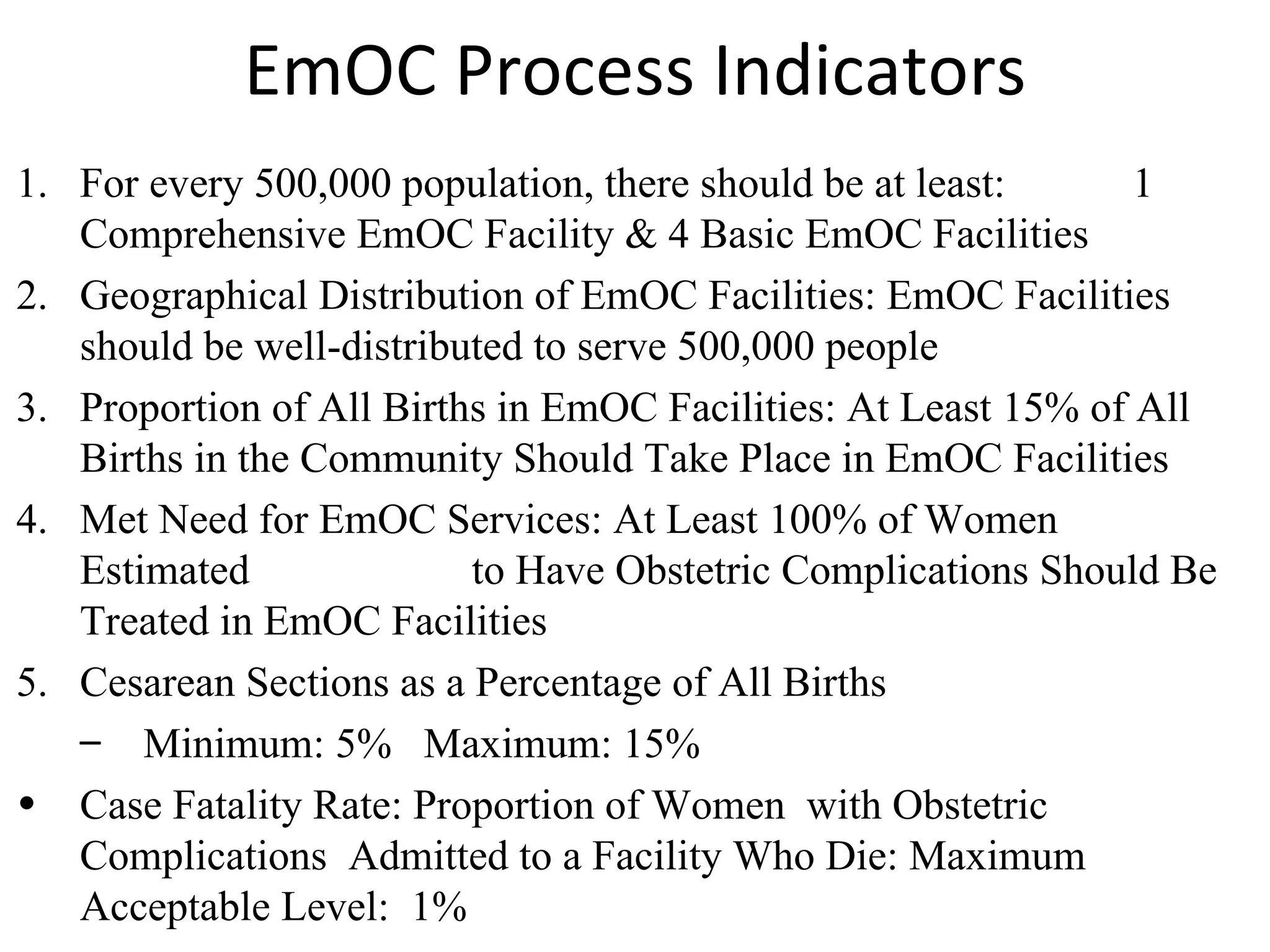
This document discusses the importance of emergency obstetric care (EmOC) in saving women's lives during pregnancy and childbirth complications. It outlines eight key EmOC functions and describes basic and comprehensive EmOC facilities. Six process indicators are presented to monitor access, utilization and quality of EmOC services, including the number of facilities per population, proportion of births at facilities, and case fatality rates. Regular monitoring of these indicators can help identify issues and guide improvements to maternal healthcare.