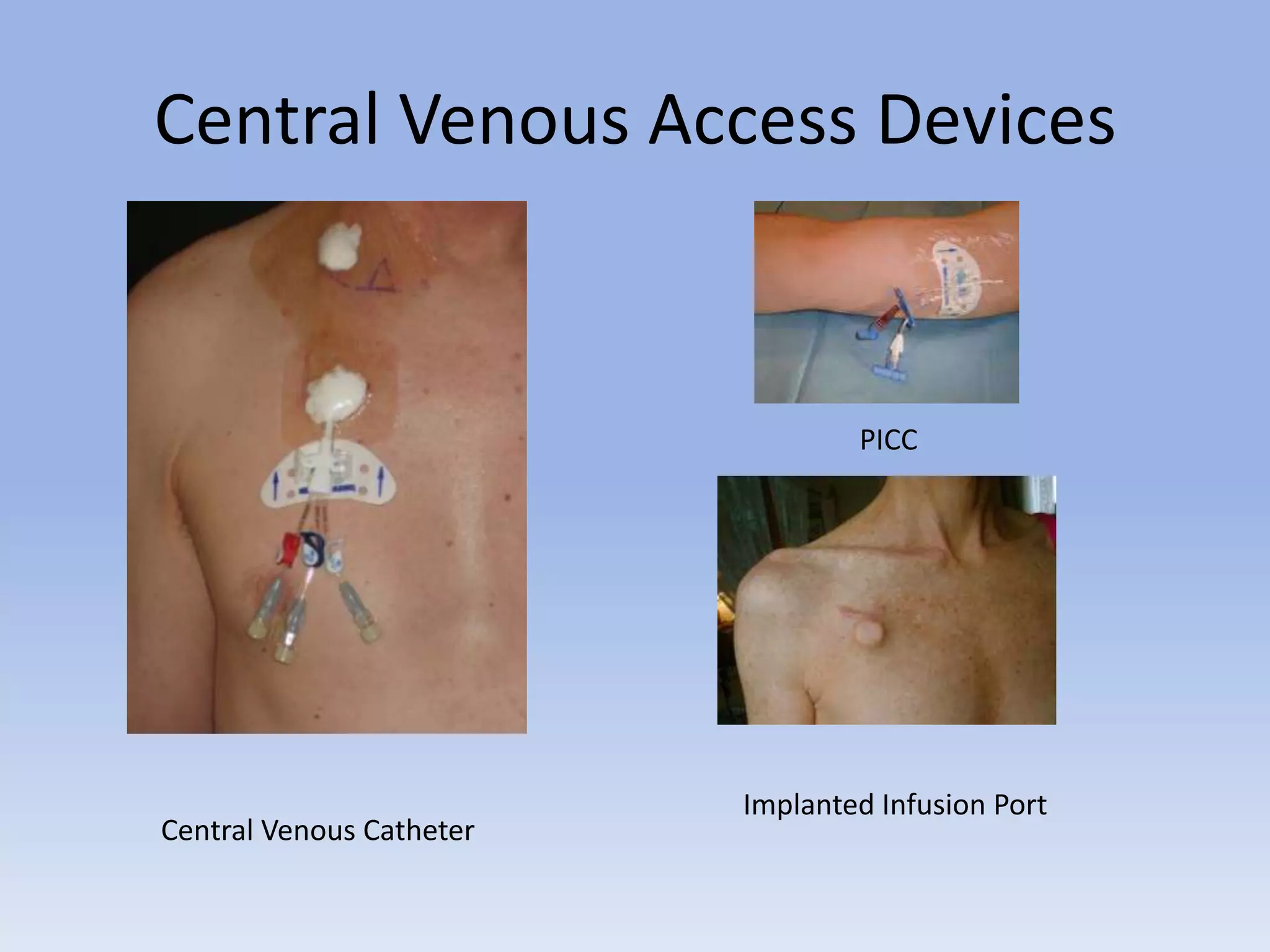
TPN is a form of intravenous nutrition given through a central line into a large vein. It provides nutrients like carbohydrates, proteins, fats, electrolytes, vitamins and minerals. TPN must be given centrally because the solutions are hyperosmolar and could damage peripheral veins. Central lines include PICCs, ports and central venous catheters. Selection depends on factors like the patient's condition and the characteristics and duration of therapy. TPN administration requires strict aseptic technique and monitoring of glucose, weight and other lab values.