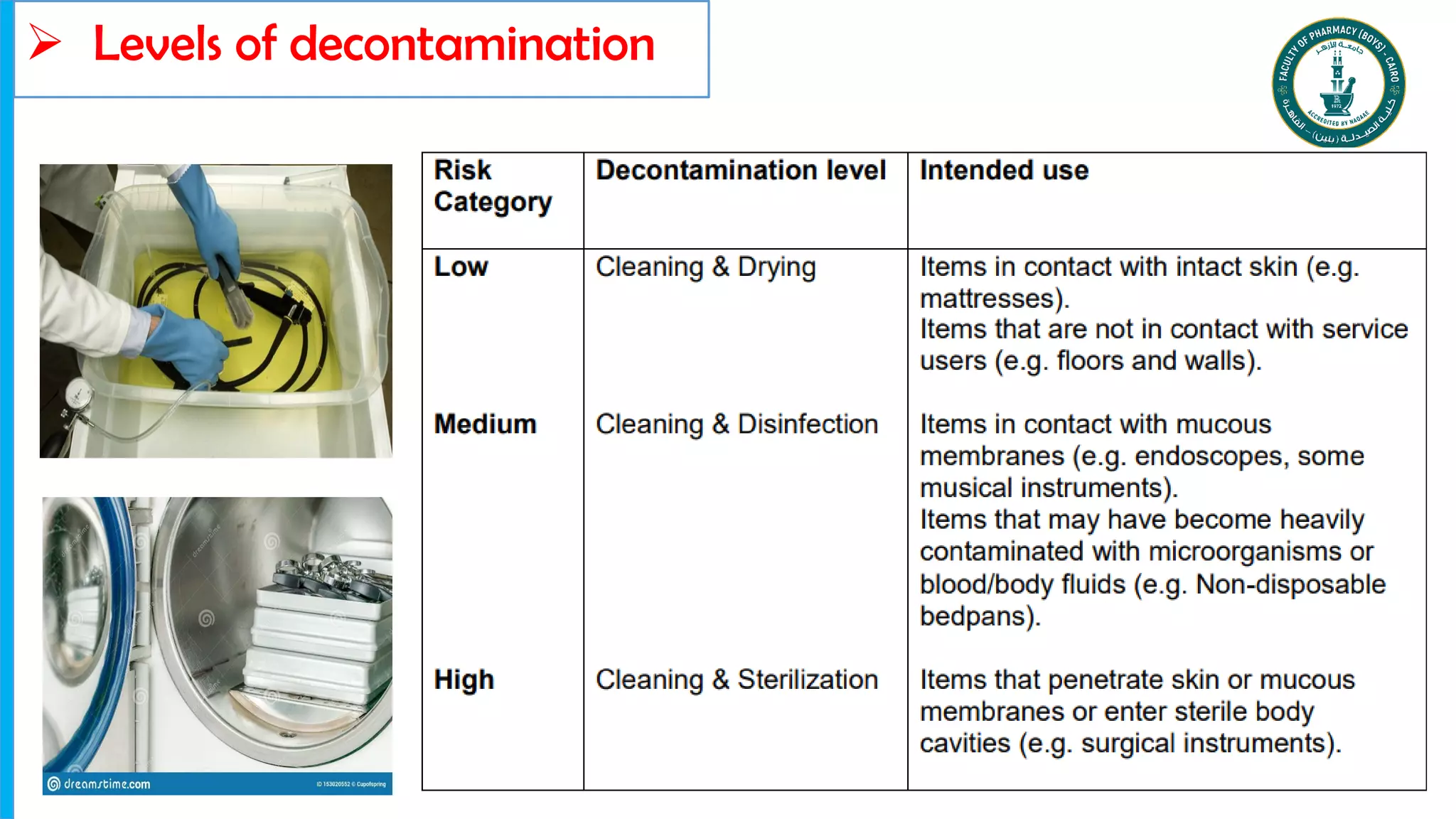
Decontamination methods for infection prevention and control were discussed, including:
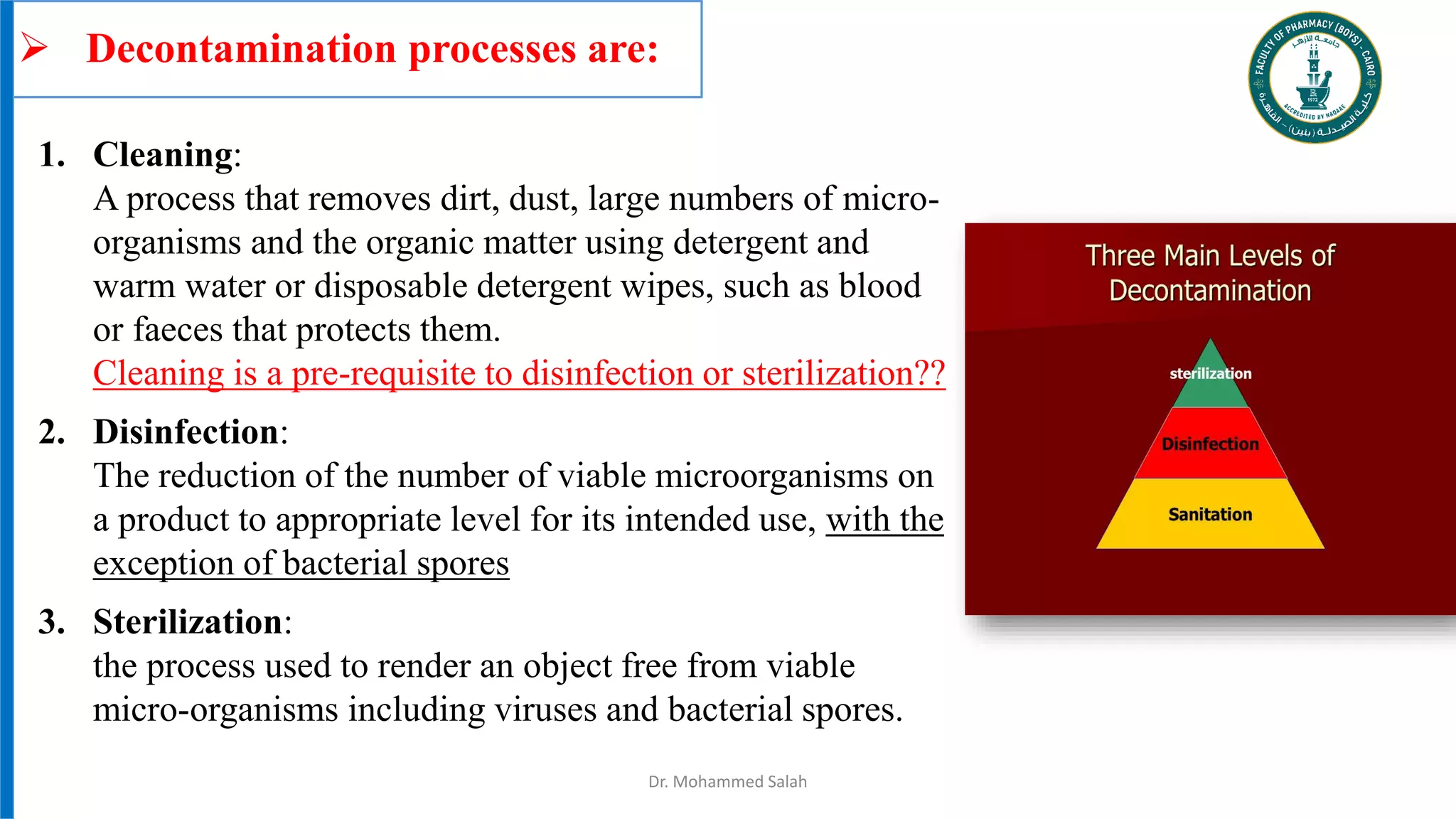
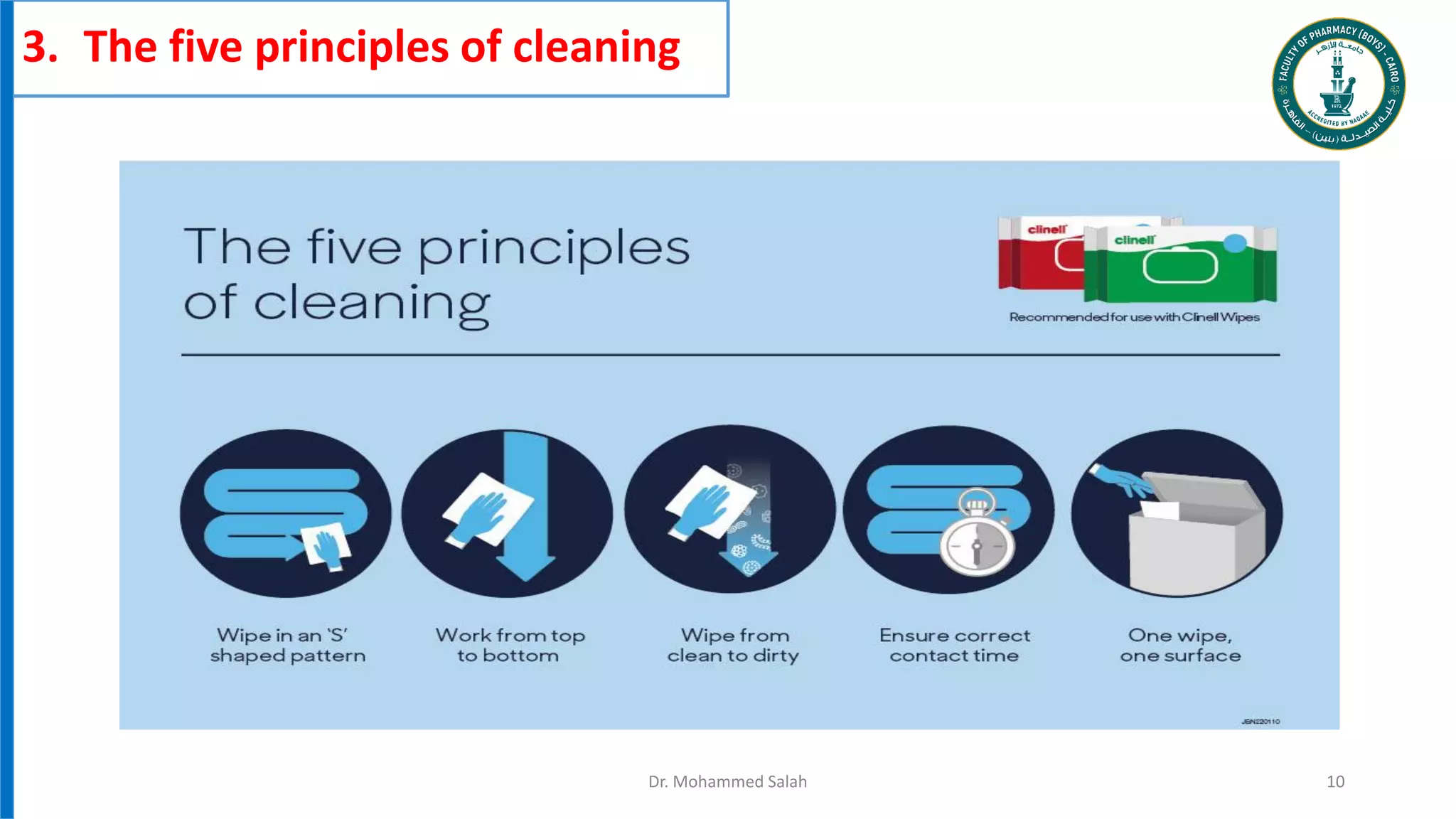
1. Cleaning removes microorganisms and organic matter using detergent and water.
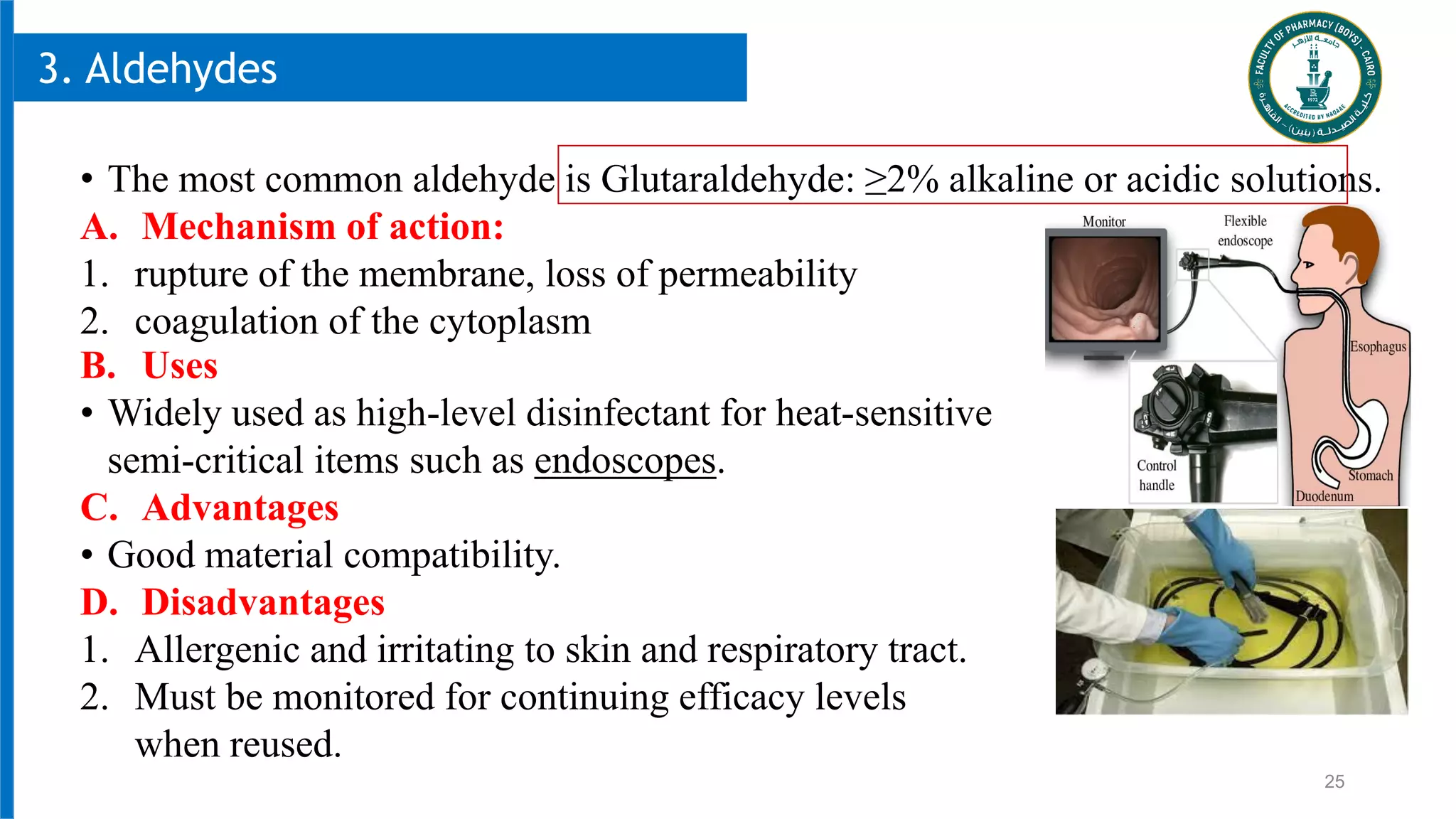
2. Disinfection reduces microorganisms to safe levels using chemicals like alcohol or chlorine compounds.
3. Sterilization uses heat, chemicals, or radiation to kill all microorganisms including bacterial spores on medical equipment to prevent infection transmission.