Bone marrow is found within bones and produces blood cells, containing two types - red marrow which produces blood cells throughout life and yellow marrow containing fat; it undergoes examination by aspiration and biopsy to evaluate blood cell production and detect abnormalities by analyzing cellular composition and bone marrow architecture.






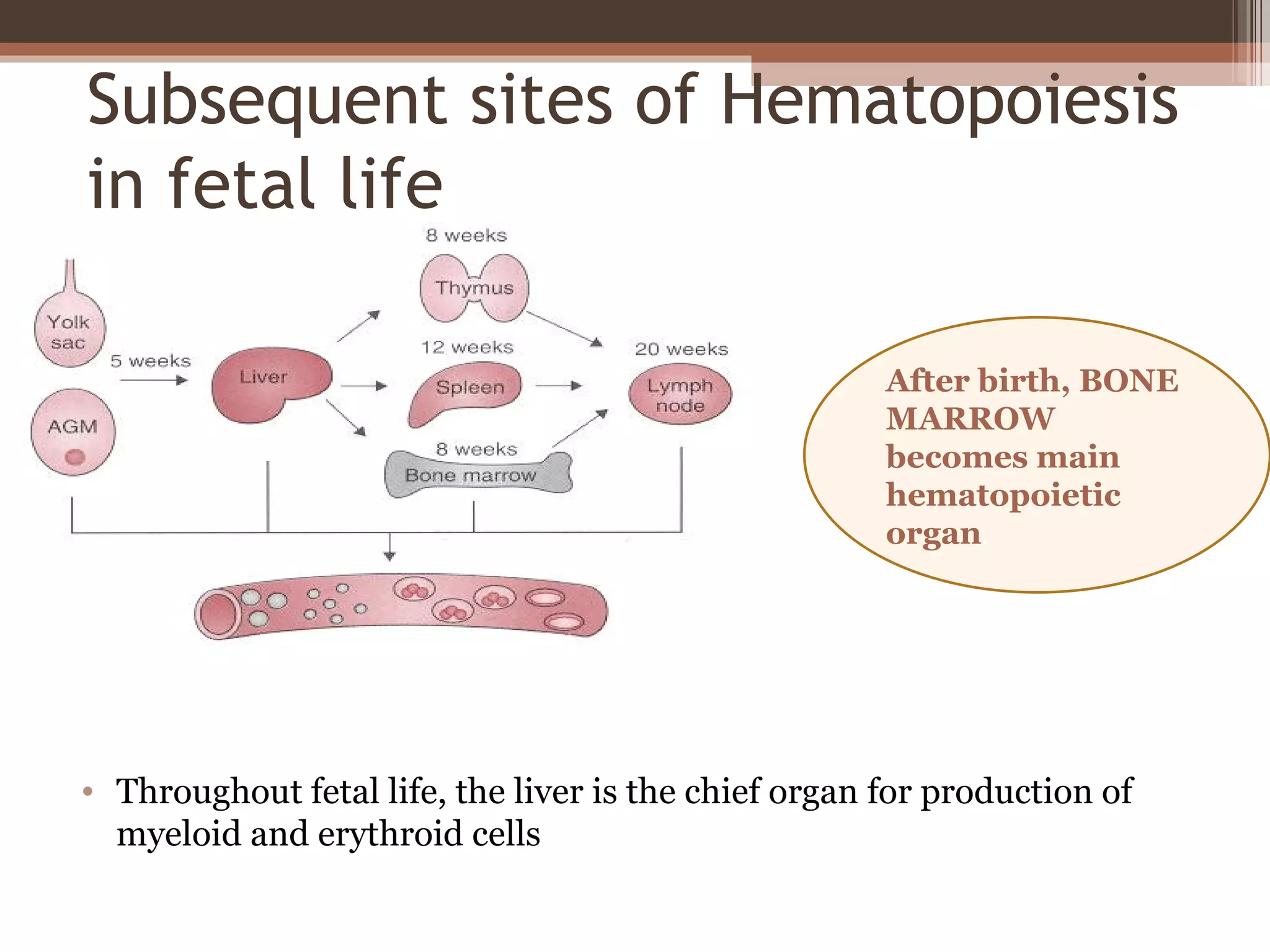














![proerythroblast
• Normal proerythroblast
[dark red arrow] in the
bone marrow. This is a
large cell with a round
nucleus and a finely
stippled chromatin
pattern. Nucleoli are
sometimes apparent.
• The cytoplasm is
moderately to strongly
basophilic.](https://image.slidesharecdn.com/bonemarrowclass-120611143149-phpapp02/75/Bone-marrow-class-24-2048.jpg)








![Normal granulocyte precursors in
the bone marrow
• Note the myeloblast
[dark red arrow] with a
high nucleocytoplasmic
ratio, diffuse chromatin
pattern and nucleolus.
• There is a promyelocyte
[green arrow] which is
larger and has a lower
nucleocytoplasmic ratio
and abundant azurophilic
granules.](https://image.slidesharecdn.com/bonemarrowclass-120611143149-phpapp02/75/Bone-marrow-class-33-2048.jpg)
































