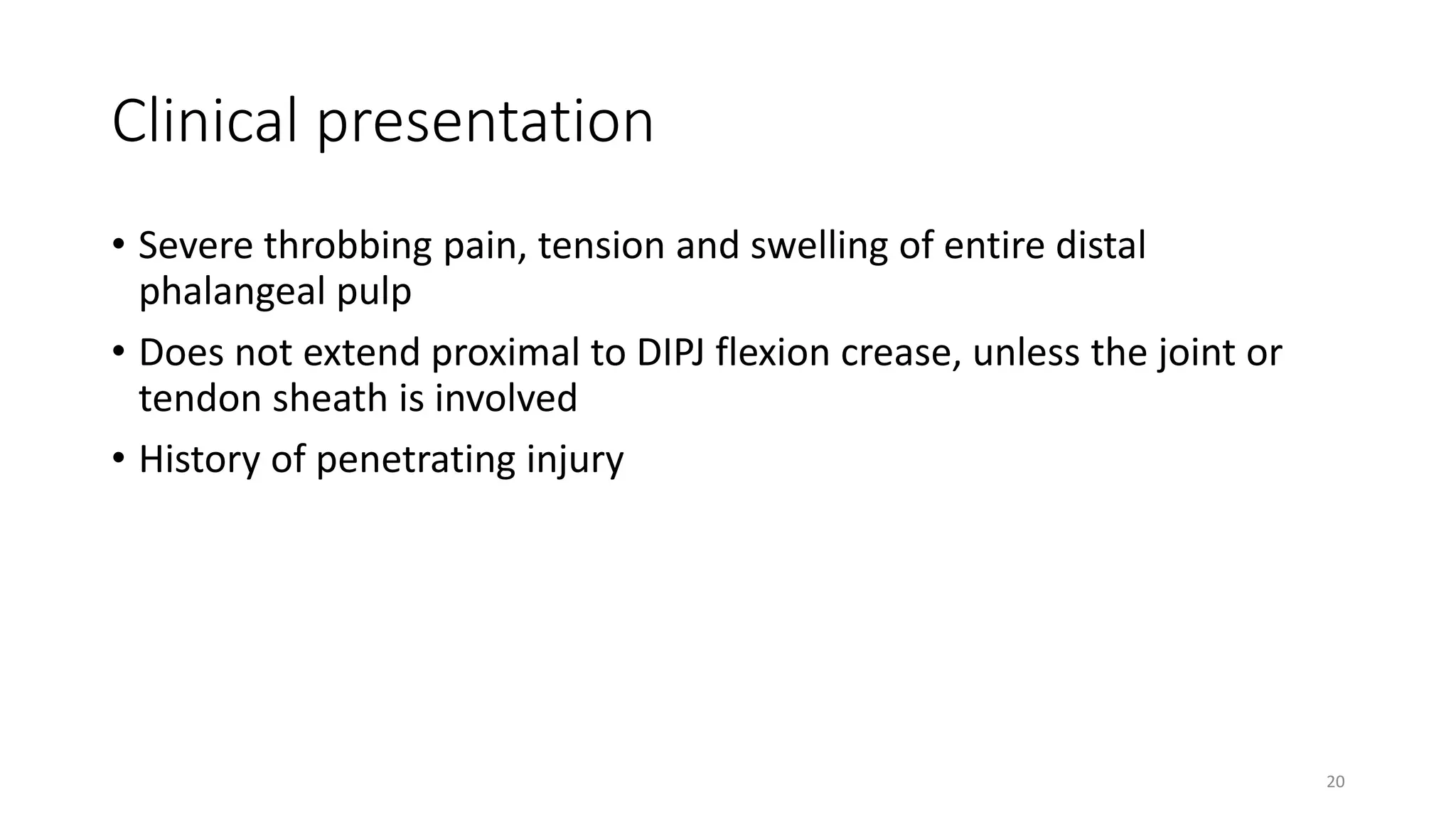
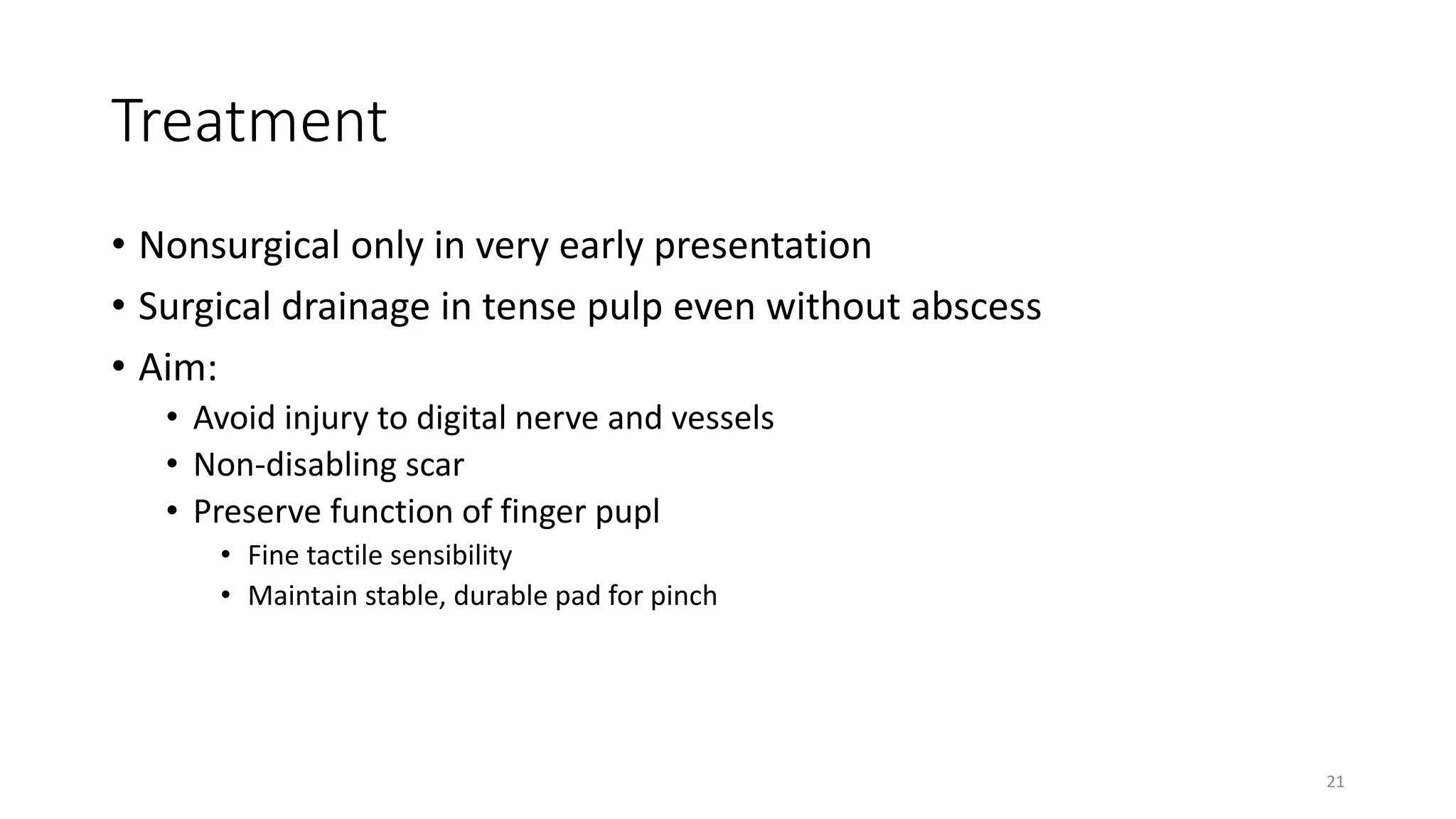
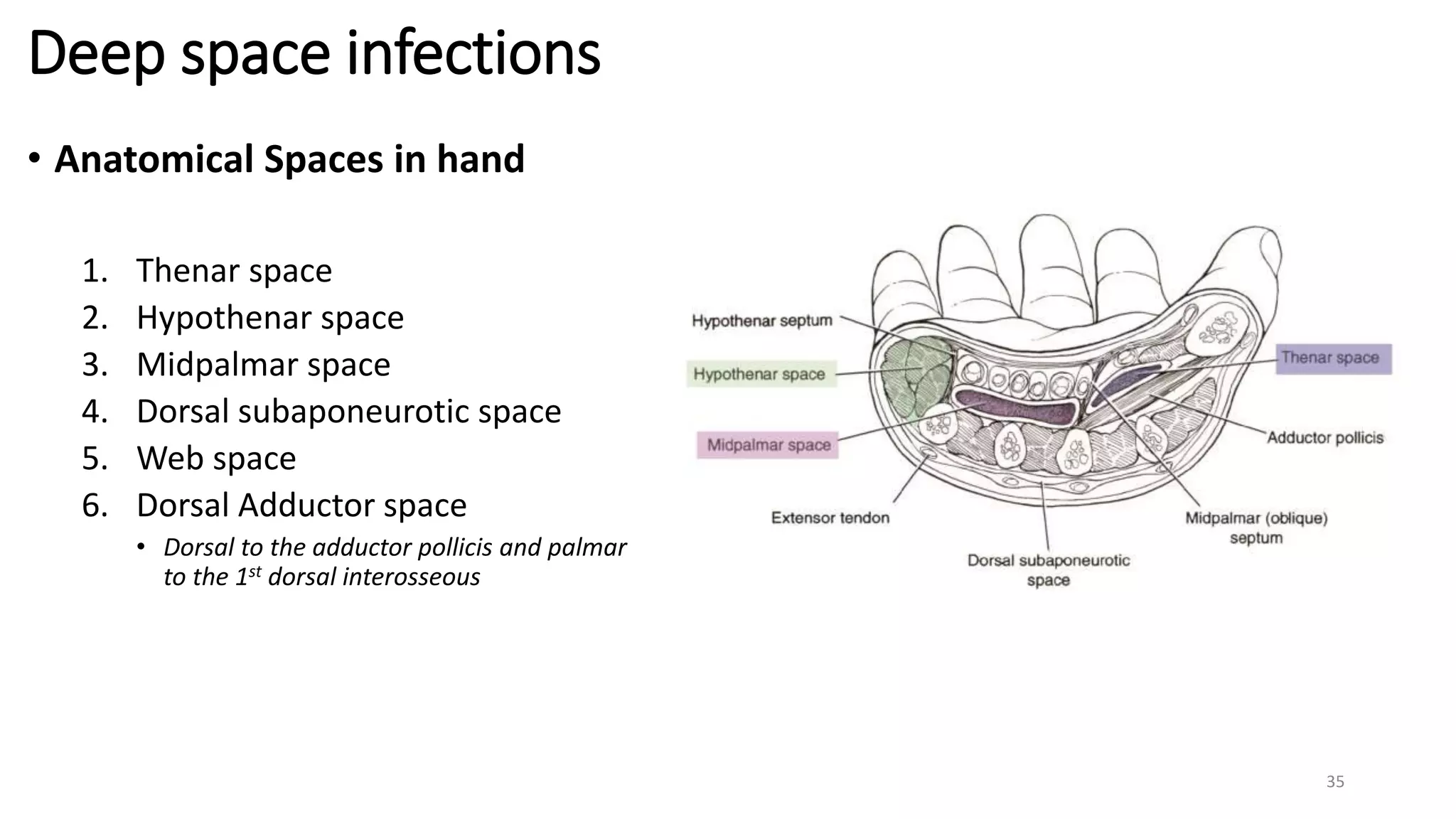
This document discusses various types of hand infections, including nail bed infections, flexor tenosynovitis, and deep space infections. It describes the anatomy, clinical presentation, treatment options, and postoperative care for each type of infection. The key points are:
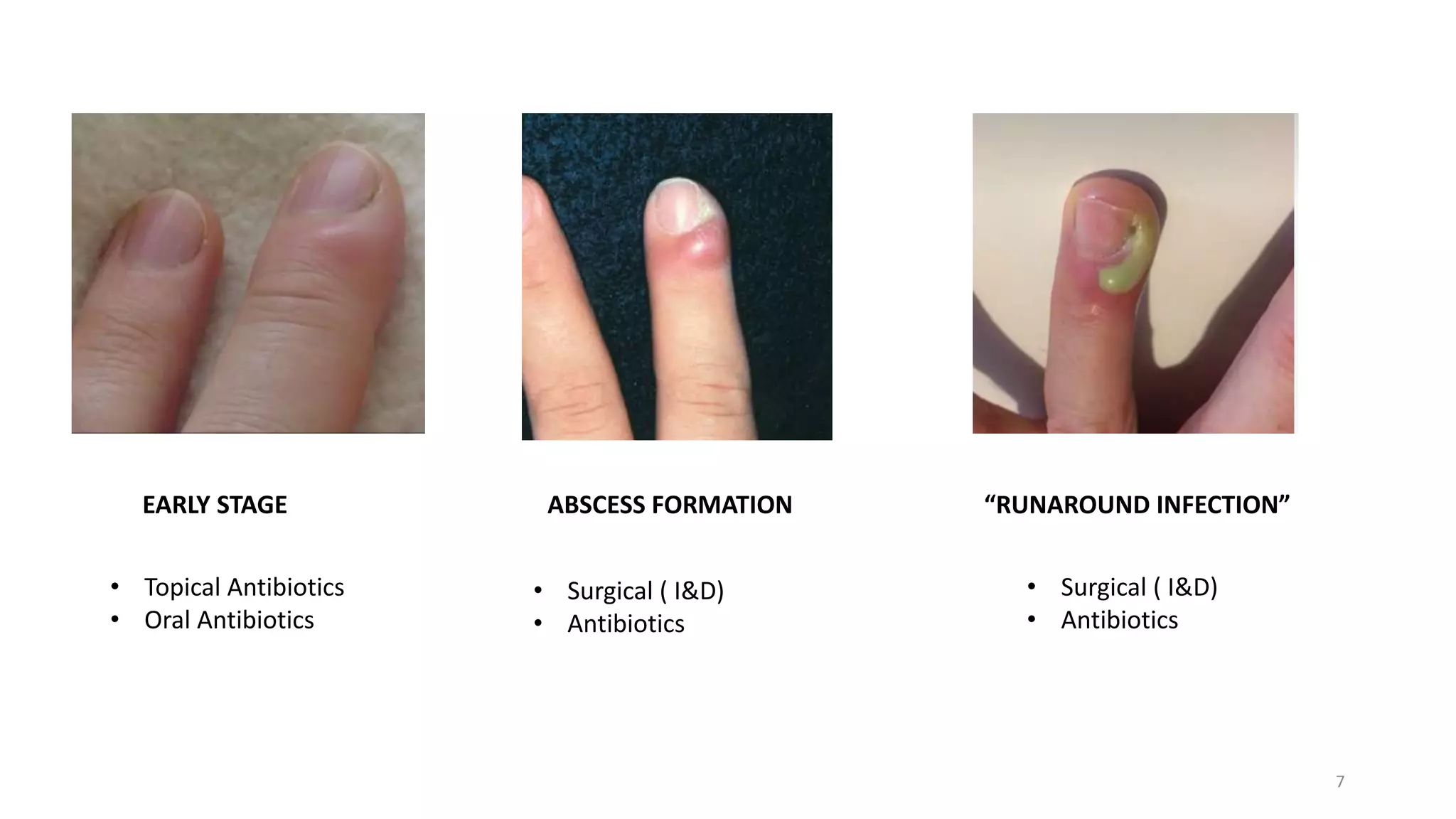
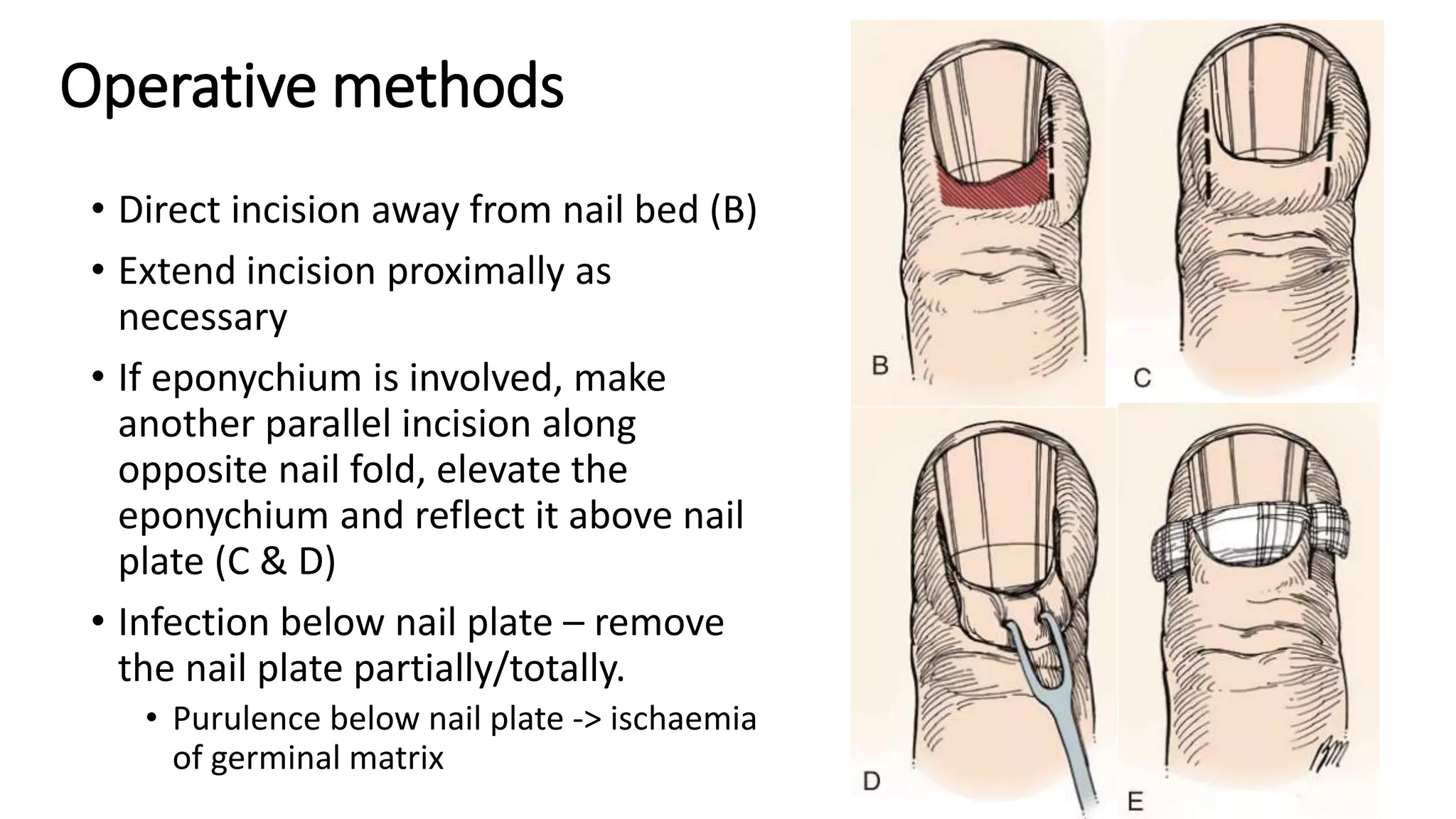
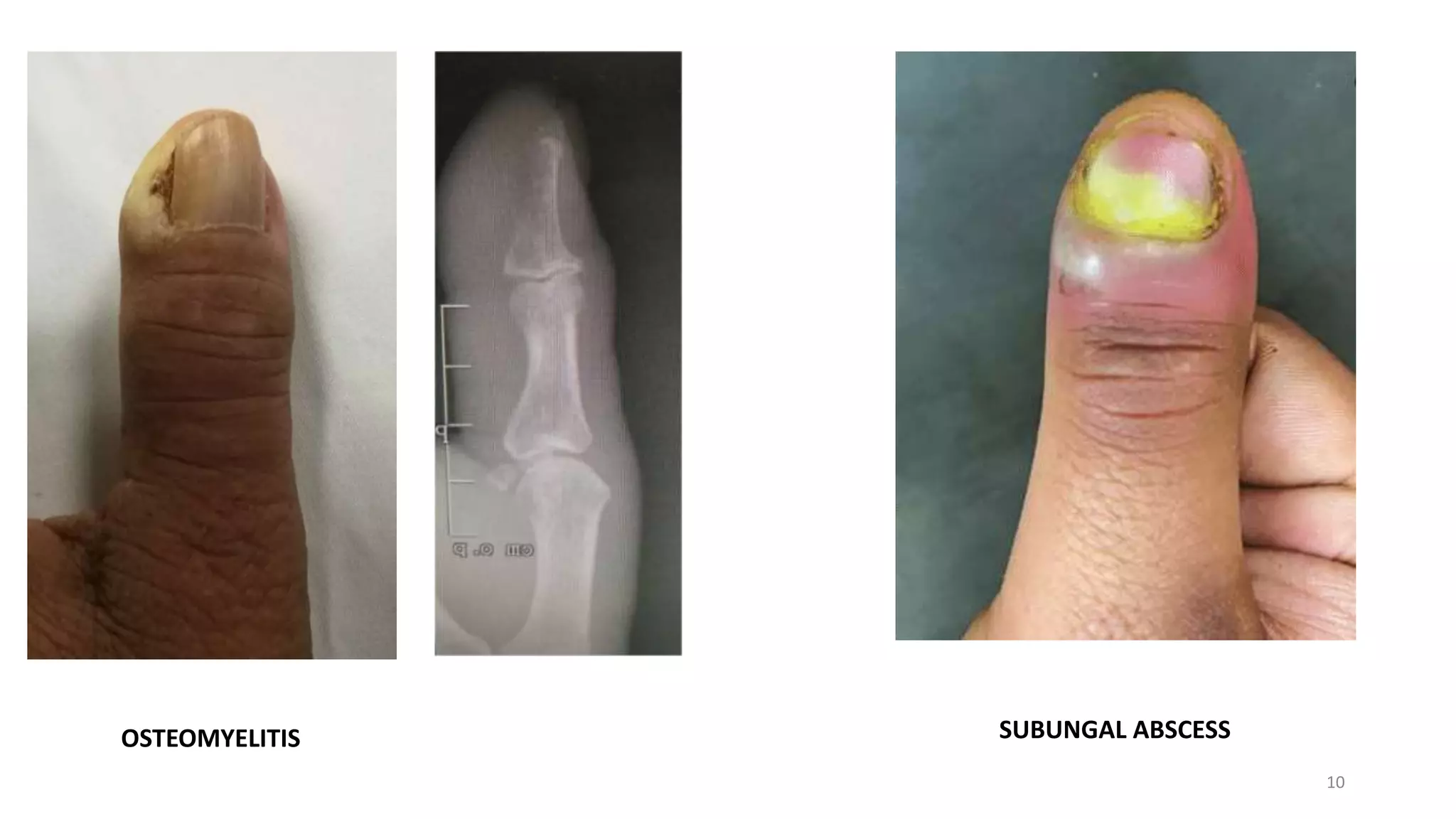
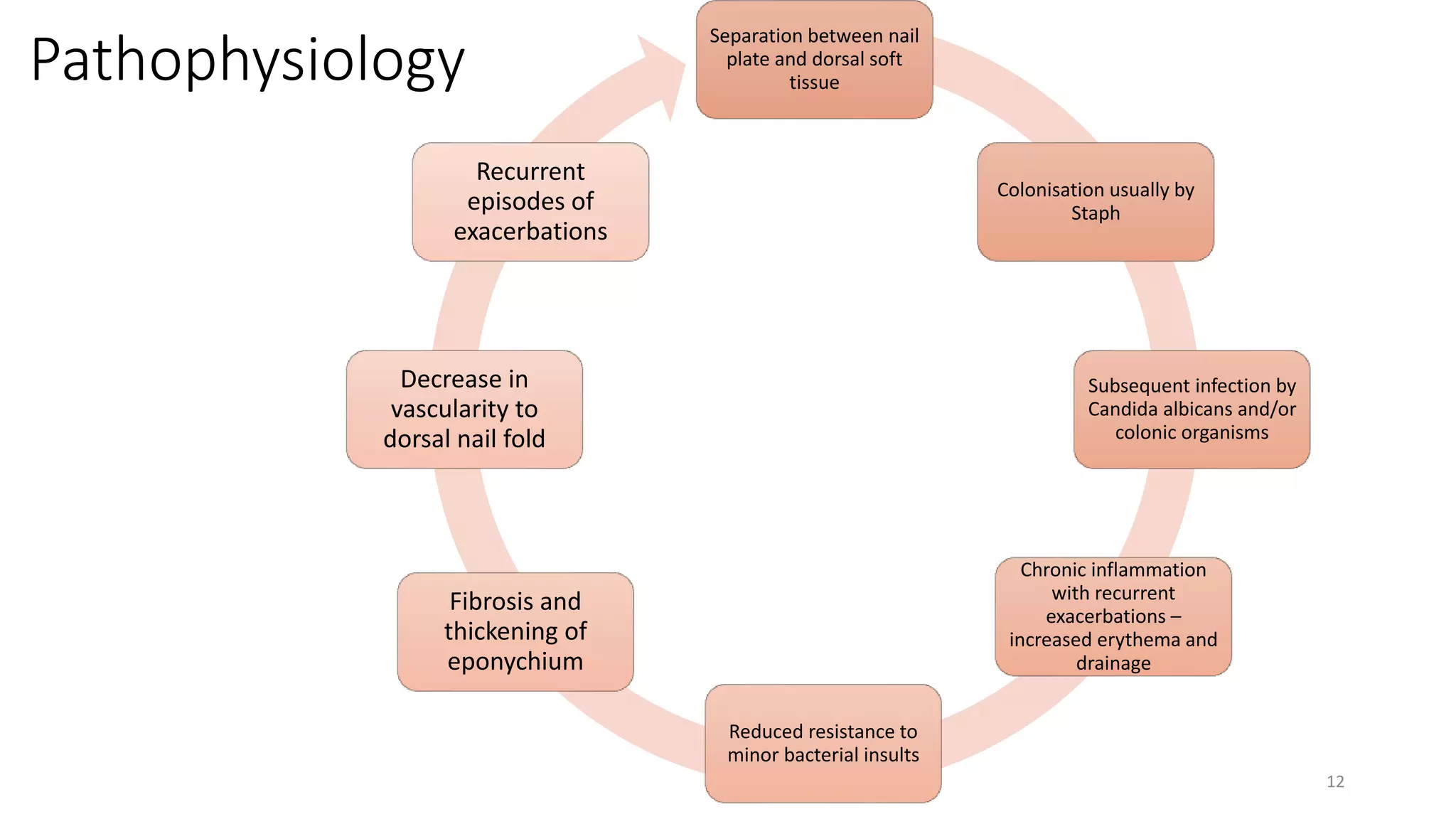
1. Nail bed infections include acute and chronic paronychia and subungal abscesses. Acute paronychia is usually caused by minor trauma and treated with antibiotics and incision/drainage if abscess forms. Chronic paronychia is more inflammatory and may require eponychial marsupialization.
2. Flexor tenosynovitis is a closed-space infection of the flexor tendon sheath