1. Blunt trauma to the eye can cause a variety of injuries depending on the force and location of impact, including direct damage to the eyeball at the point of impact, damage from compression waves transmitted through the eye's fluid contents, and indirect damage from impact with bony eye socket structures.
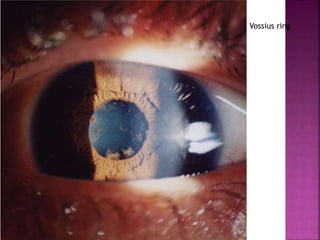
2. Specific injuries include abrasions, tears or detachments of the cornea, iris, retina, choroid or sclera, hyphema, cataracts, subluxation or dislocation of the lens, vitreous hemorrhages, glaucoma, commotio retinae, retinal tears and detachments, and macular holes.
3. More severe blunt trauma can cause