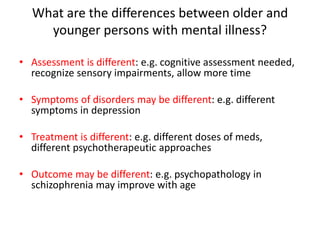
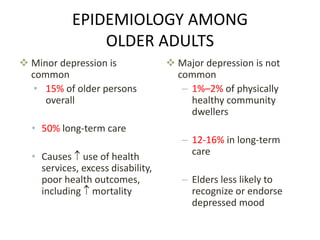
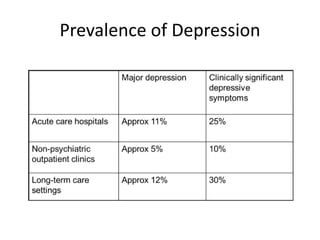
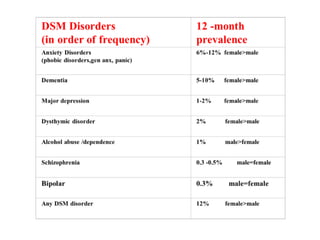
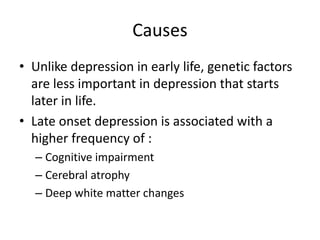
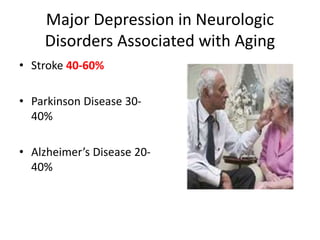
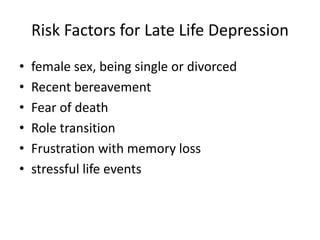
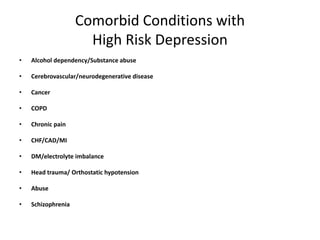
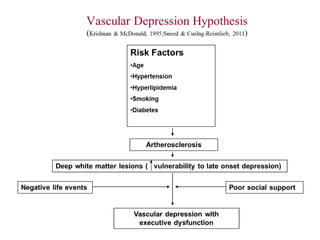
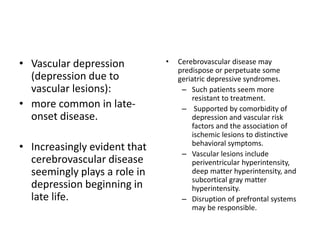
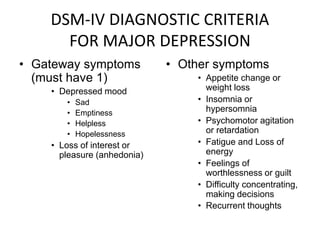
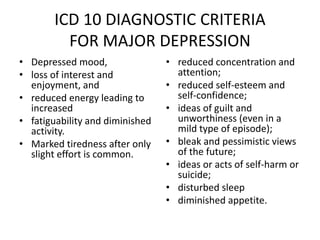
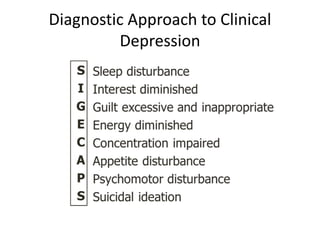
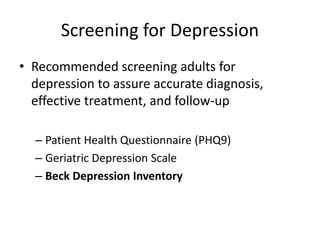
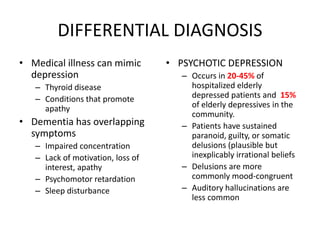
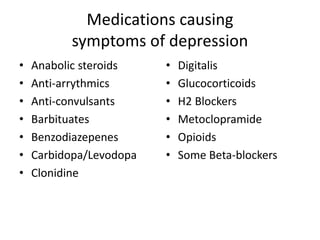
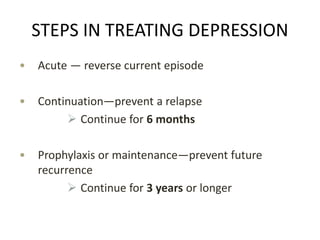
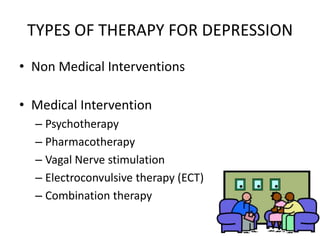
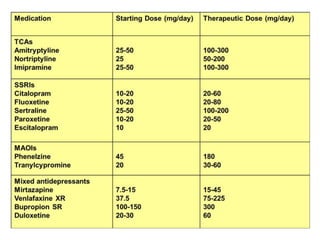
Depression is common among elderly individuals and can be caused by medical illnesses, bereavement, stressful life events, and cognitive impairment. Major depression affects 1-2% of healthy older adults and 12-16% of those in long-term care. Late-life depression is often underrecognized and undertreated. Screening tools can help diagnose depression according to DSM-IV or ICD-10 criteria, and treatment involves both pharmacological and non-pharmacological approaches aimed at the acute episode, preventing relapse, and long-term prophylaxis. Differential diagnosis considers medical and psychiatric conditions.