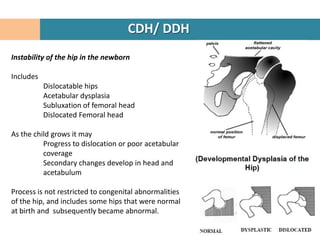
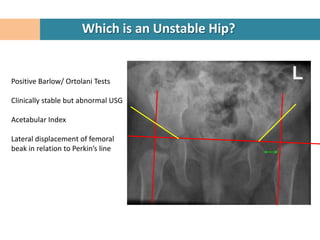
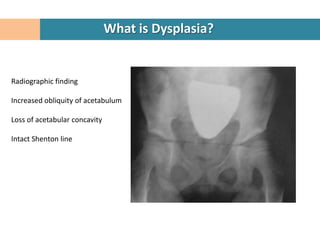
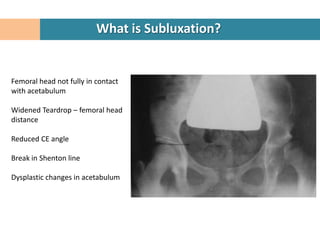
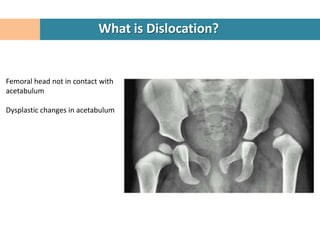
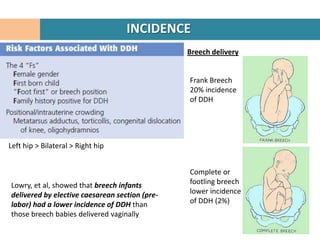
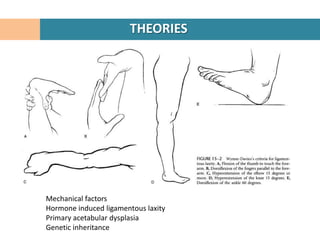
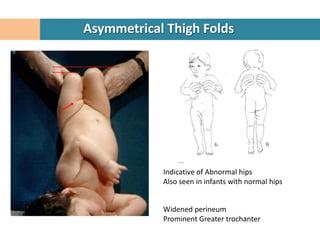
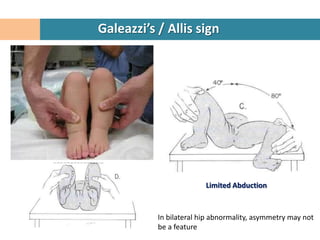
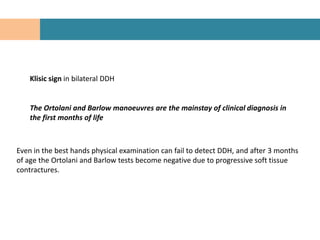
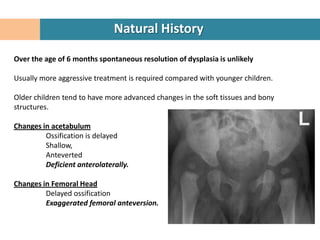
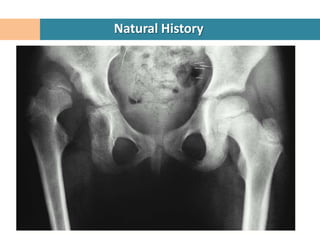
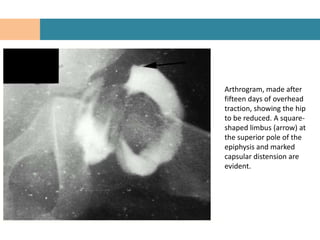
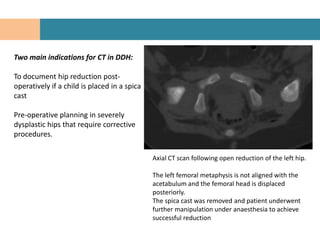
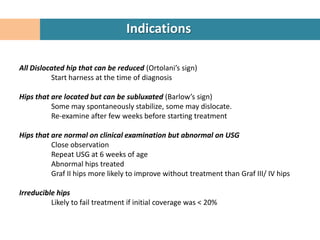
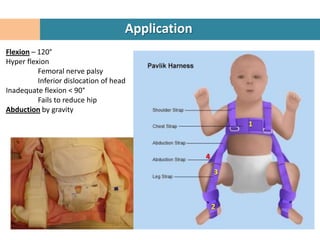
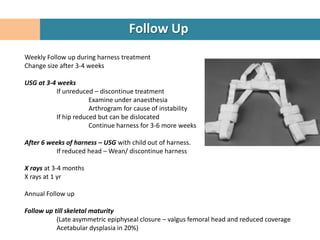
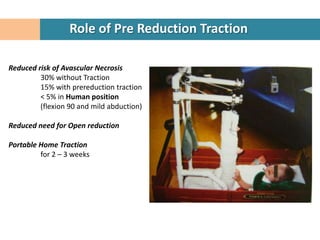
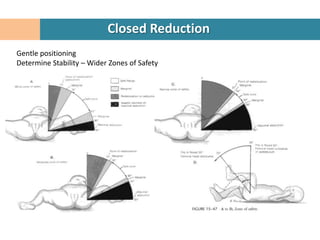
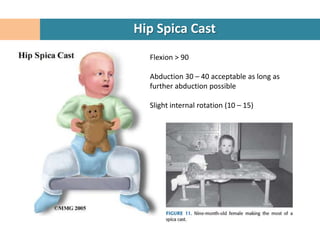
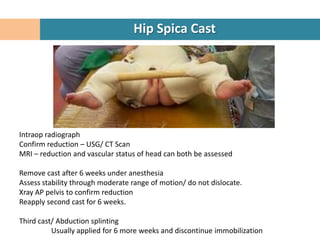
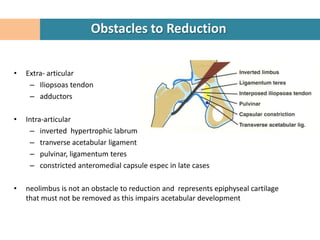
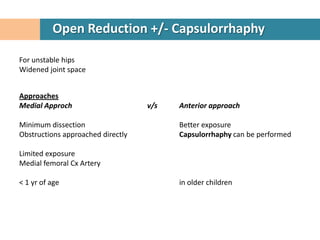
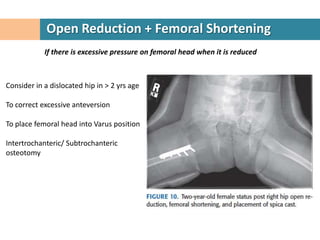
The document discusses developmental dysplasia of the hip (DDH), including: definitions; clinical detection from birth to 6 months using tests like Ortolani's and Barlow's; treatment from birth to 6 months using a Pavlik harness or closed reduction and hip spica casting; and treatment from 6 to 18 months also using closed reduction and hip spica casting, with the goal of obtaining and maintaining reduction without damaging the femoral head. Obstacles to reduction like hypertrophic soft tissues are also mentioned.