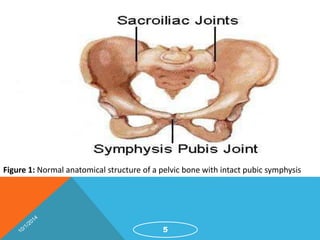
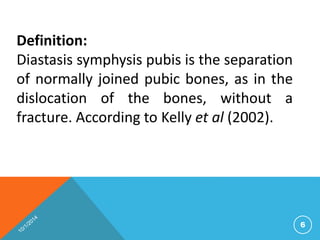
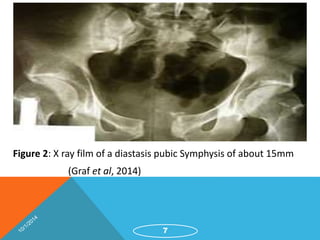
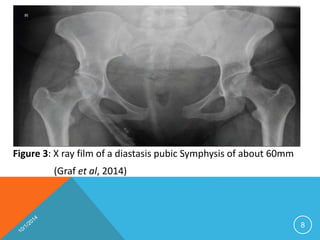
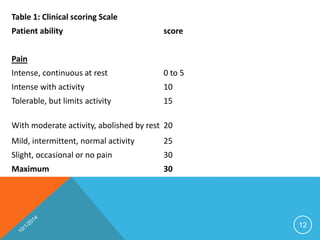
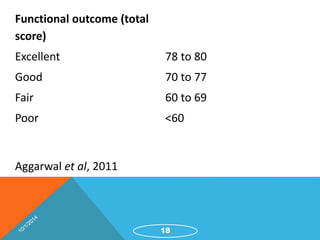
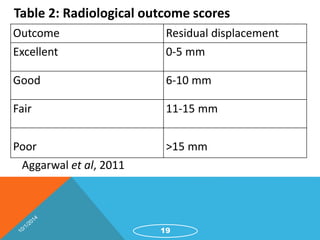
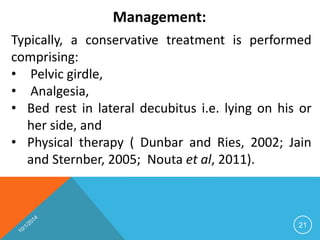
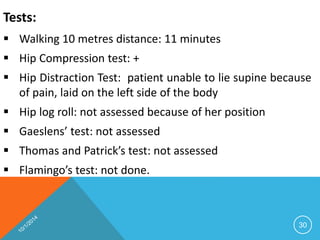
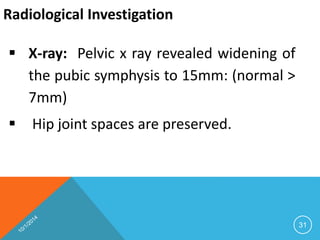
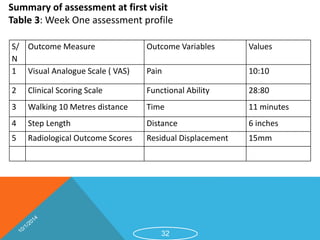
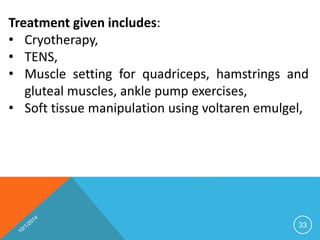
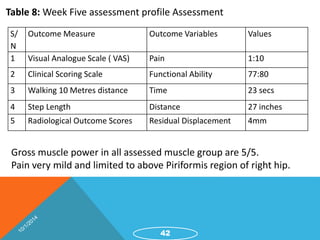
This document discusses the management of diastasis pubic symphysis, beginning with an introduction to the condition, epidemiology, etiology, assessment, management, prognosis, and a case study. Diastasis pubic symphysis is defined as the separation of normally joined pubic bones without fracture. It is most commonly caused by pregnancy and delivery. Assessment involves pelvic x-rays and pain/functional scales. Conservative management includes pelvic support, physical therapy, and medications. Prognosis is typically good if addressed promptly with proper management. A case study demonstrates successful treatment of a woman's severe diastasis pubic symphysis over 5 weeks using these conservative approaches.