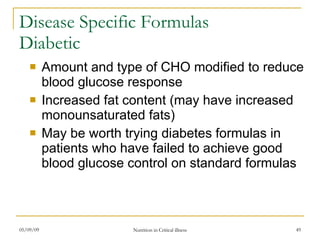
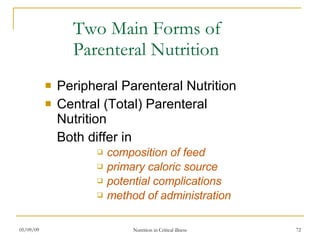
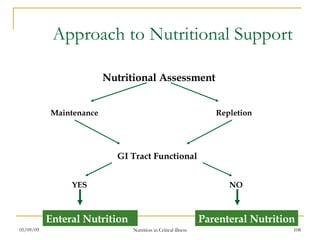
The document provides an overview of nutritional support in critical illness, including definitions, history, assessment, guidelines, and types of nutrition support such as enteral and parenteral nutrition. It discusses screening patients, performing nutritional assessments, determining caloric and protein needs based on stress level and condition, selecting appropriate enteral formulas, initiating and managing enteral feeds, and ordering and administering parenteral nutrition including determining fluid volumes, electrolytes, and other additives.