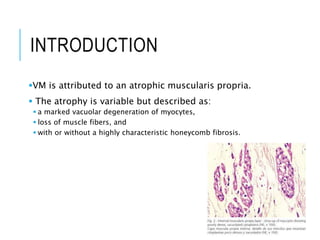
Visceral myopathy is a rare inherited condition characterized by impaired function of smooth muscle cells in the intestines and sometimes bladder. It is caused by atrophy of the muscularis propria layer. Patients may experience a range of gastrointestinal symptoms including nausea, vomiting, abdominal pain and distension. Diagnosis involves ruling out other causes of bowel obstruction and confirming muscle degeneration on histopathology. Treatment focuses on fluid resuscitation, gastric/colonic decompression and in some cases parenteral nutrition or surgery. The condition can be difficult to diagnose due to non-specific symptoms and similarity to other gastrointestinal diseases.