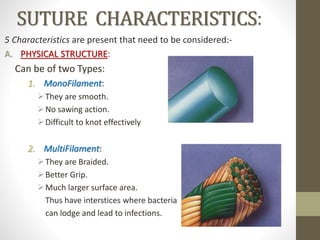
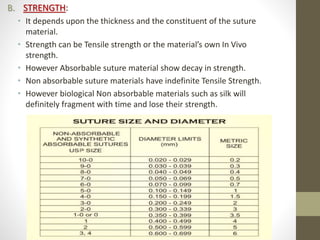
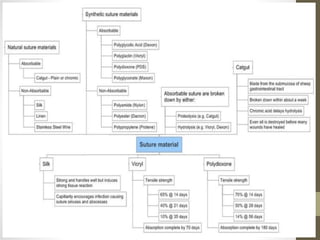
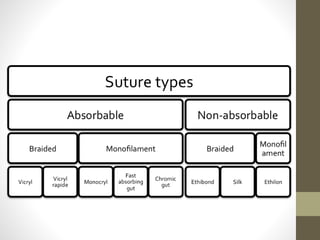
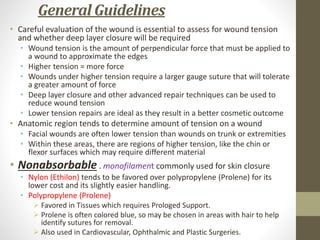
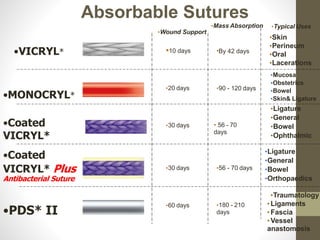
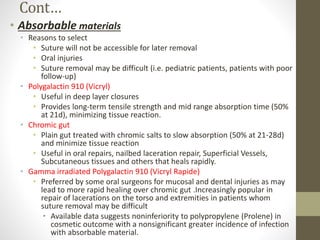
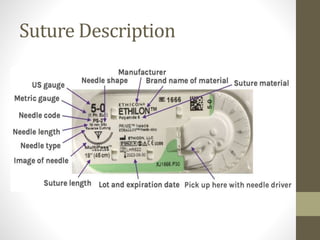
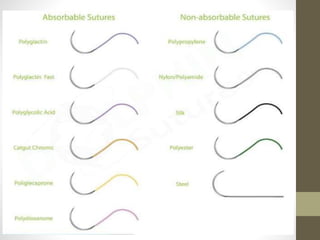
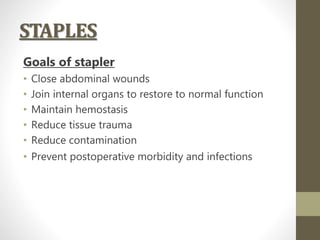
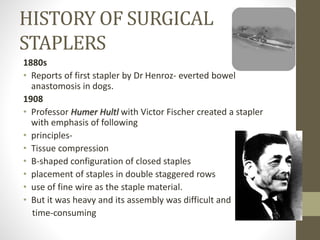
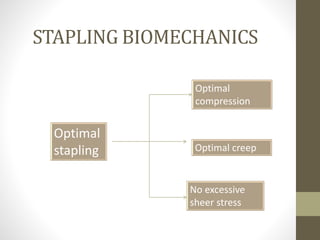
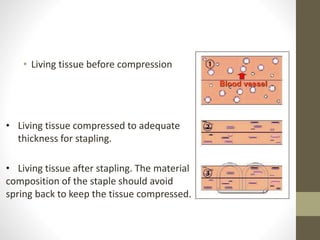
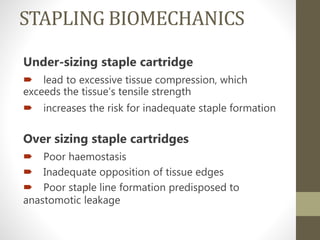
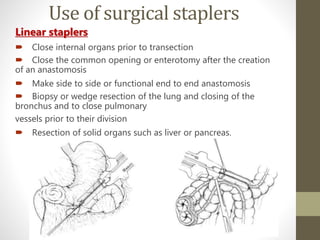
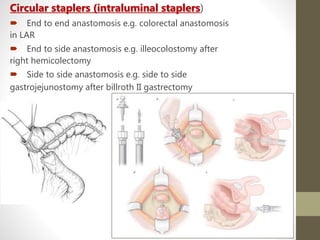
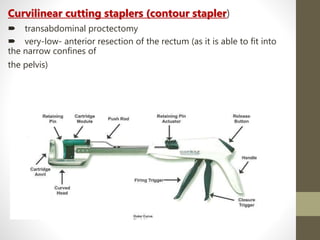
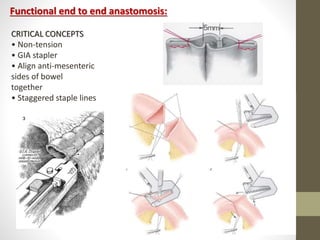
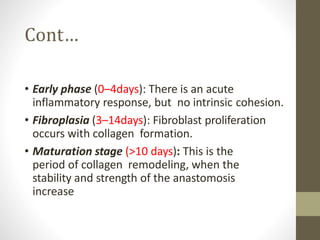
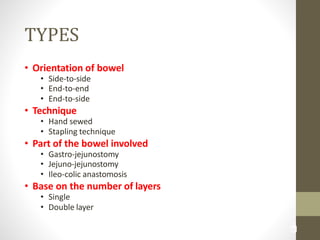
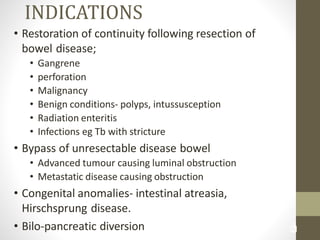
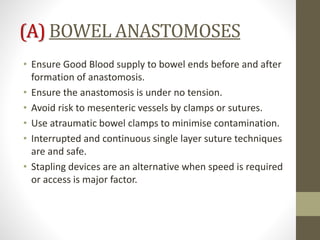
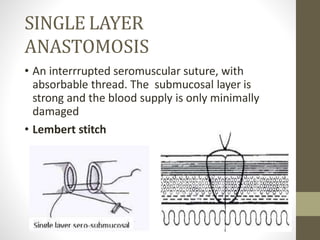
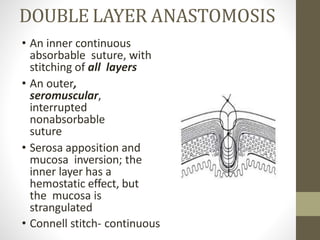
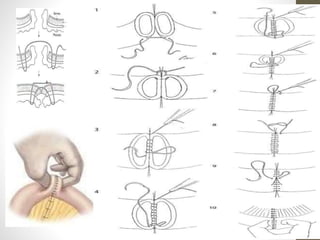
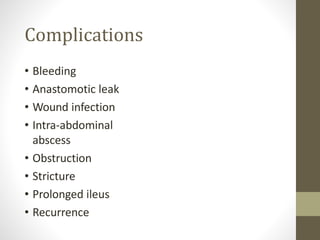
This document provides an overview of suture materials and staplers. It discusses the history and characteristics of various suture materials, including absorbability, tensile strength, and tissue reaction. Key suture materials mentioned include Vicryl, Monocryl, PDS, and Prolene. The document also covers stapler types including linear and circular staplers. Principles of anastomosis are discussed, including indications, healing phases, and techniques such as single-layer and double-layer anastomoses for bowel and vascular anastomoses. Complications of anastomoses like bleeding, leak, and stricture are also summarized.