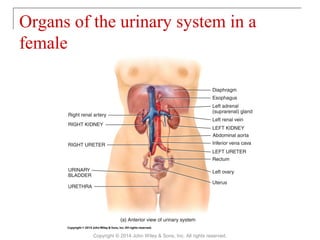
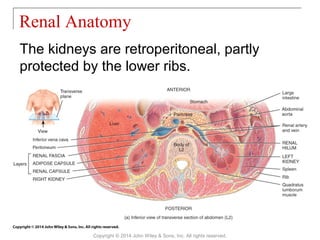
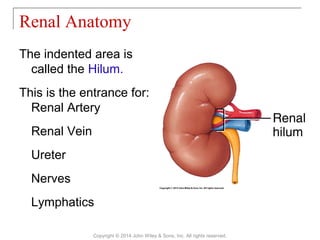
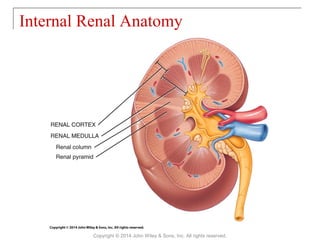
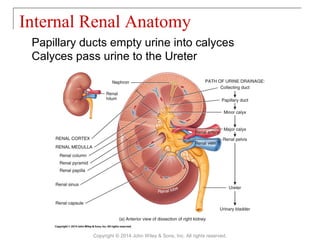
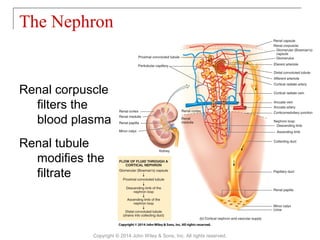
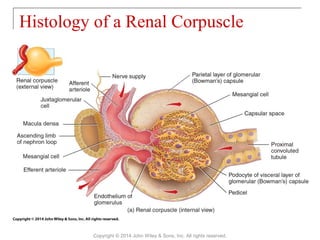
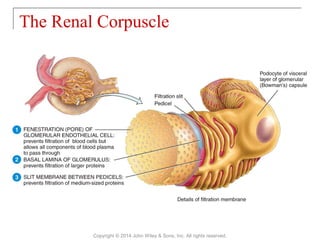
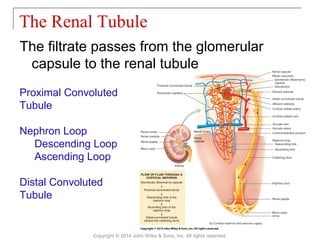
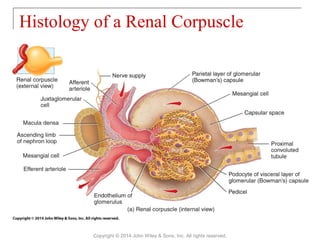
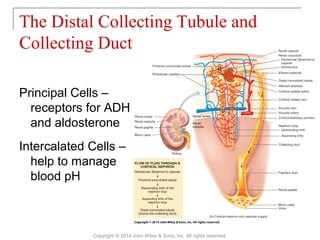
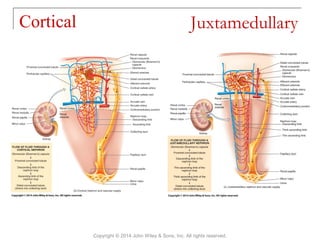
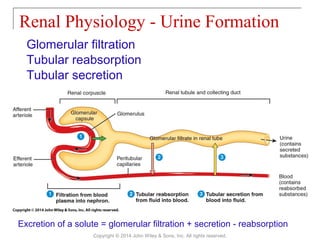
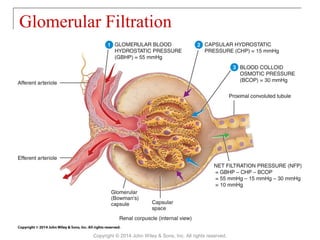
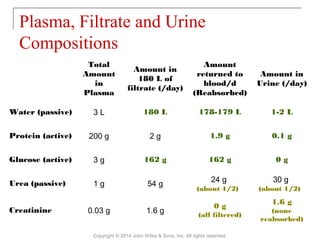
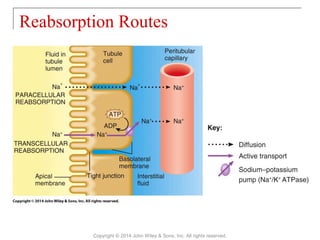
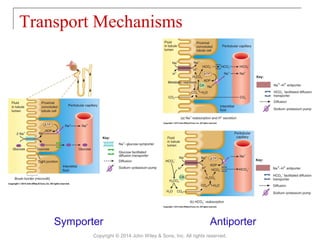
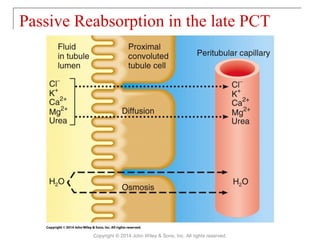
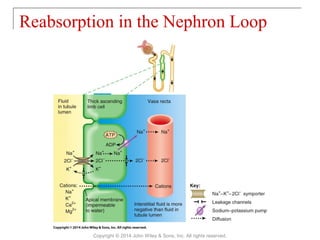
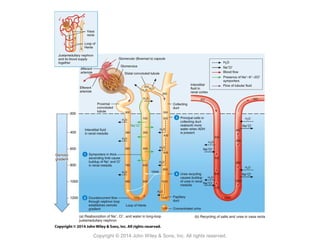
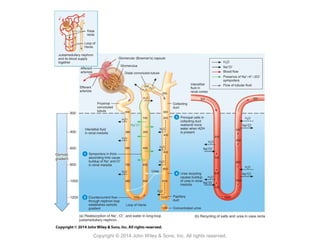
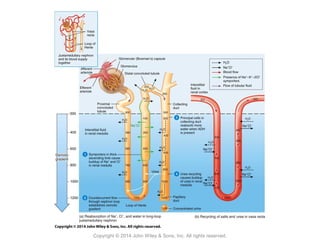
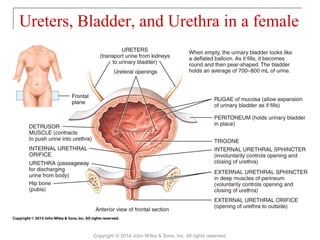
The document summarizes key aspects of kidney and urinary system anatomy and physiology. It describes how the kidneys, along with the ureters, bladder, and urethra, work together to maintain fluid homeostasis and remove wastes from the blood. Key functions of the kidneys include regulating blood volume, pressure, pH, and ion concentrations through glomerular filtration, tubular reabsorption and secretion. The nephron is the functional unit of the kidney, consisting of the renal corpuscle and renal tubule.