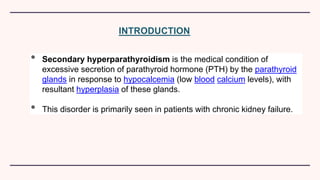
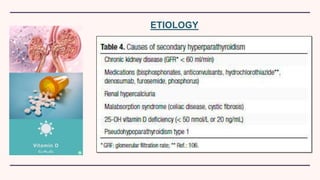
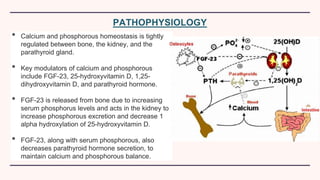
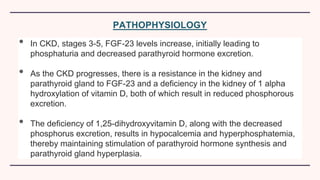
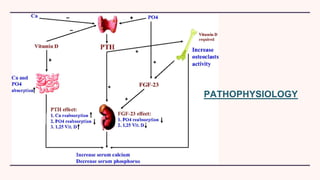
Secondary hyperparathyroidism is characterized by excessive parathyroid hormone secretion due to hypocalcemia, primarily seen in chronic kidney failure patients. The condition results from disruptions in calcium and phosphorus balance, leading to parathyroid gland hyperplasia and various clinical manifestations. Management includes dietary phosphate restrictions, vitamin D supplementation, and potential parathyroidectomy if hormone levels remain high despite treatment.