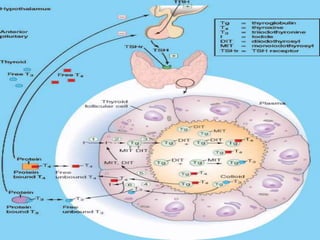
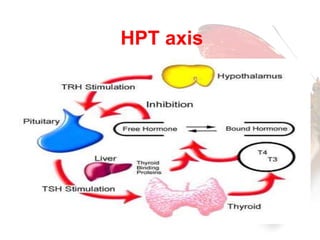
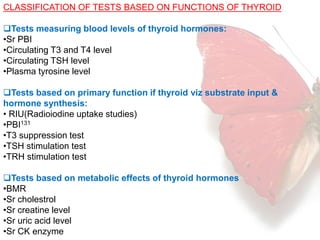
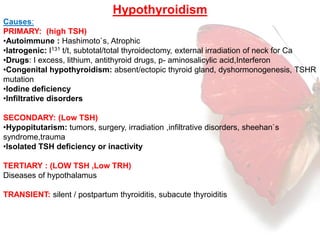
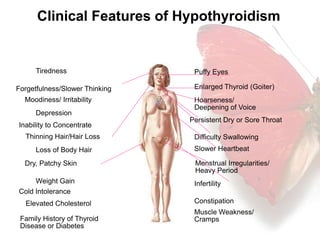
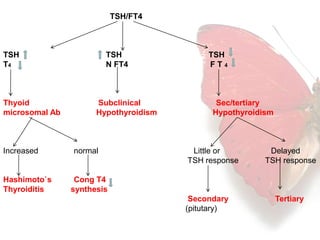
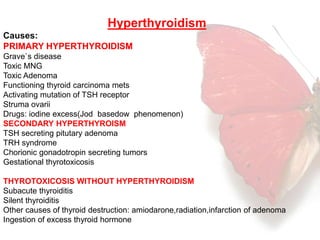
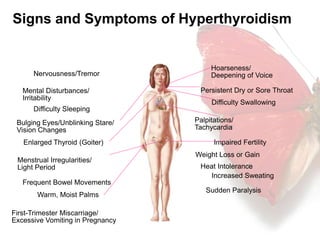
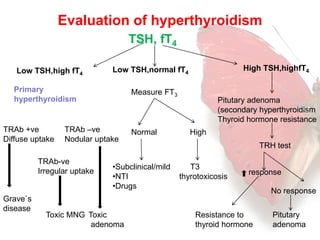
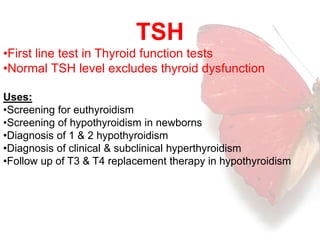
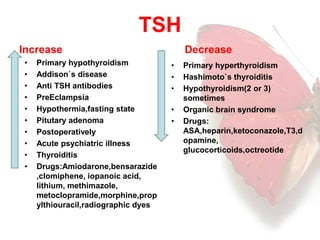
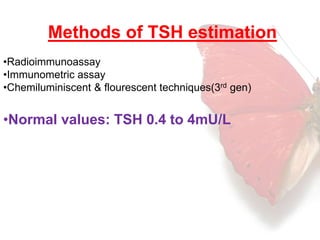
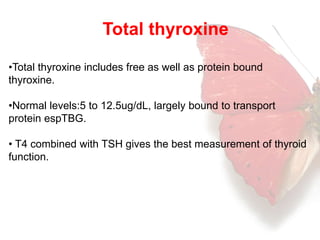
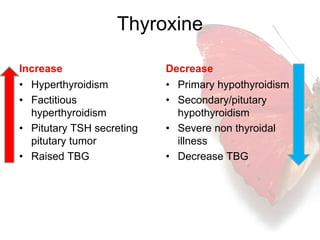
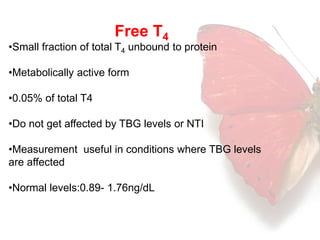
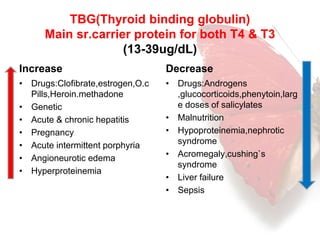
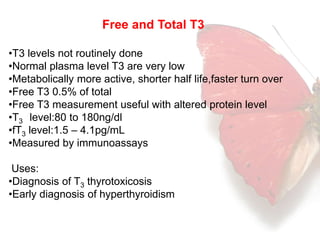
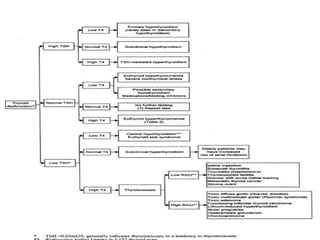
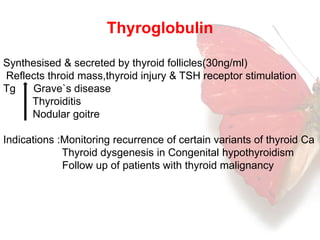
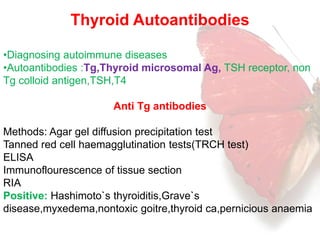
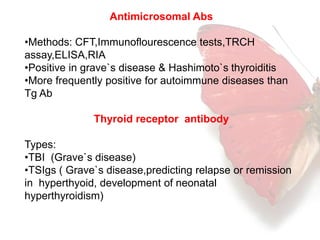
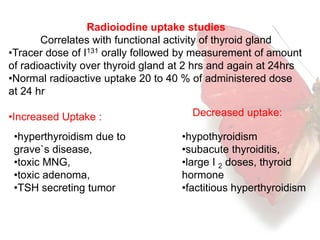
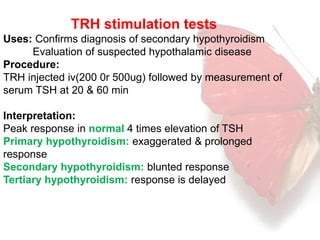
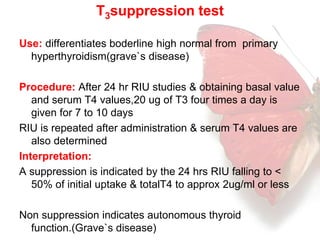
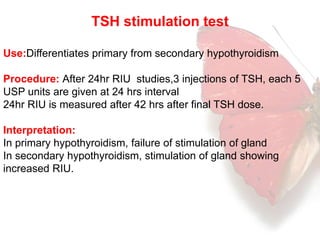
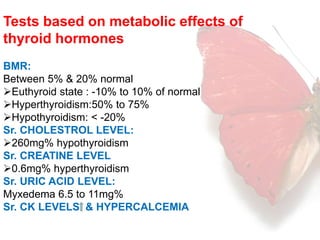
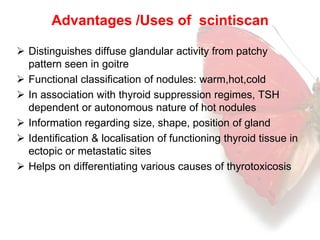
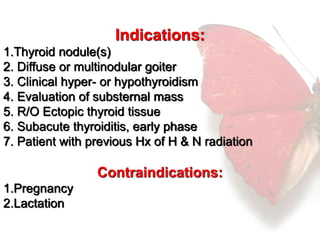
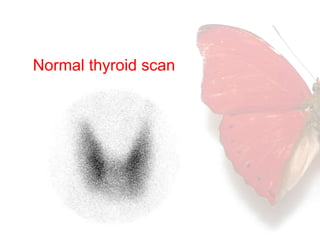
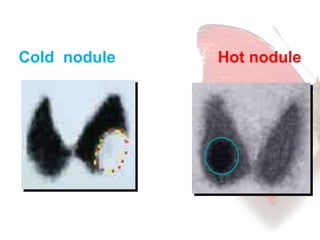
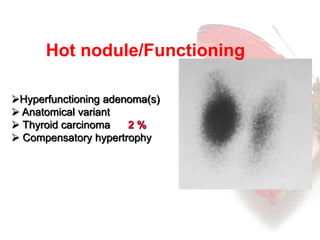
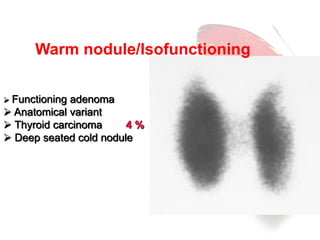
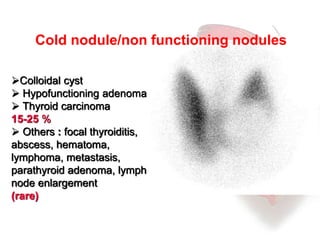
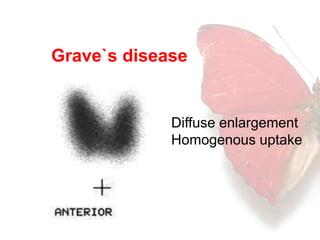
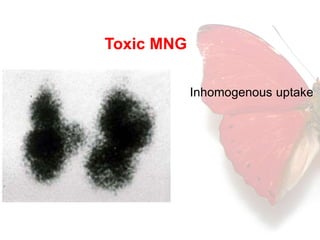
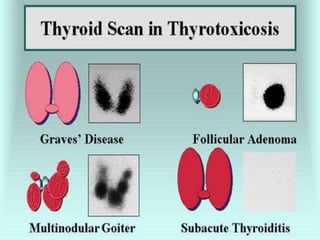
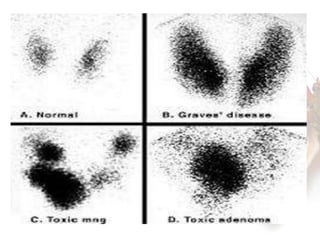
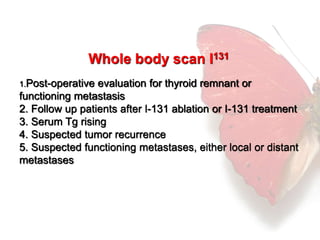
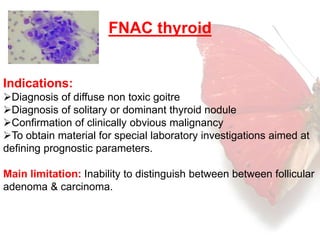
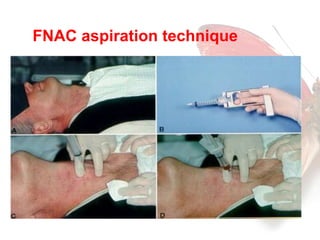
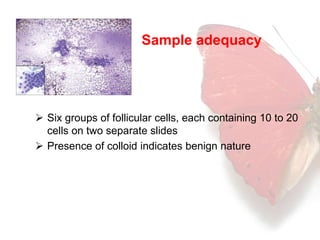
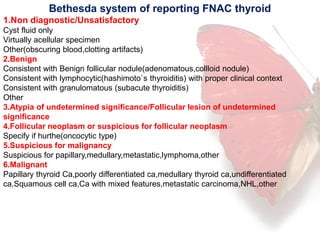
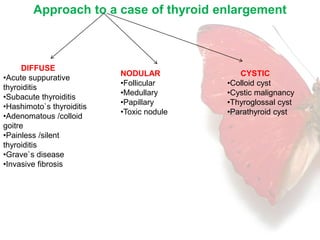
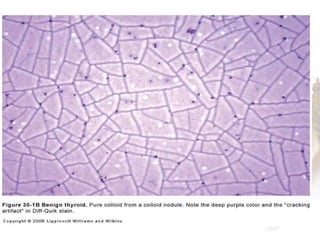
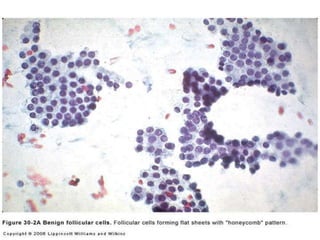
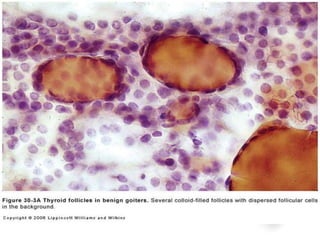
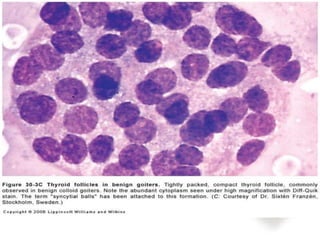
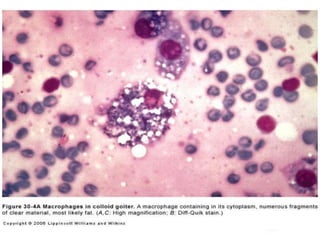
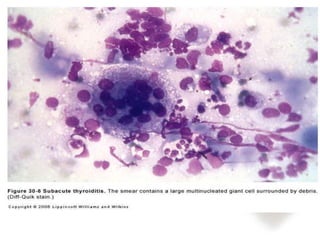
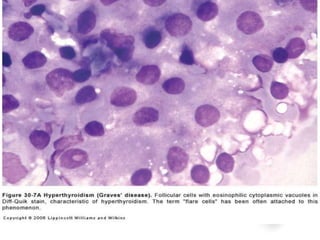
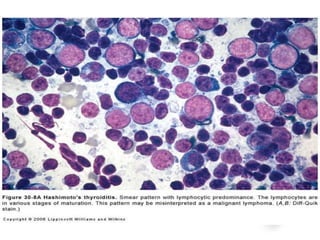
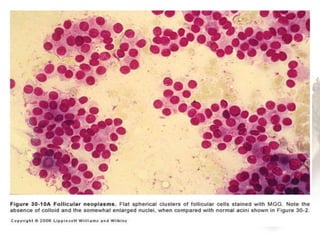
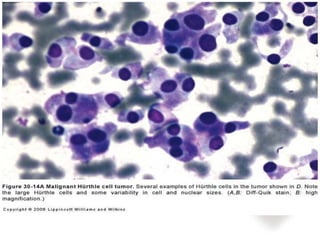
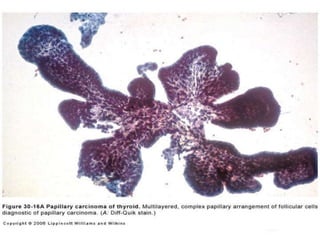
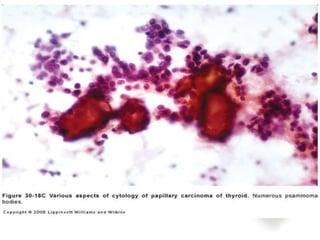
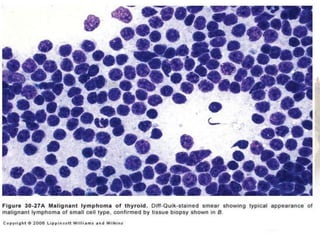
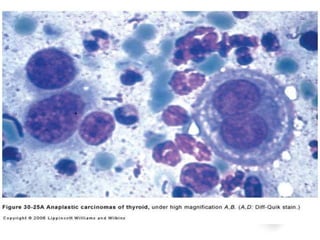
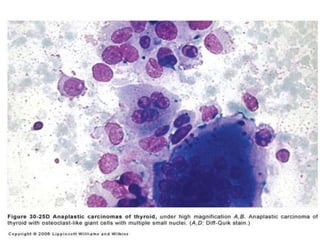
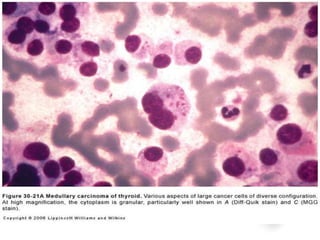
This document discusses thyroid function tests. It provides a classification of thyroid tests based on measuring hormone levels, thyroid function, metabolic effects, and detecting autoimmune diseases. Common tests described include TSH, free T4, T3, thyroid antibodies, radioactive iodine uptake, TRH stimulation, and thyroid scanning. Abnormalities in thyroid function testing can indicate hypothyroidism or hyperthyroidism. The document outlines causes and clinical features of each, and how to evaluate results based on hormone levels. Fine needle aspiration cytology of the thyroid is also summarized.