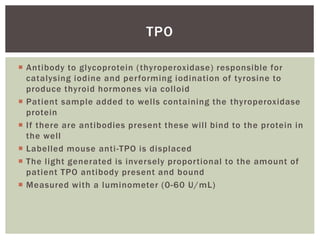
This document discusses thyroid autoantibodies, which are antibodies that mistakenly attack the thyroid gland. It begins by describing the thyroid and thyroid hormones. It then discusses different types of thyroid disease such as hypothyroidism, which includes Hashimoto's disease, and hyperthyroidism, which includes Graves' disease. The main thyroid autoantibodies - TPO, TRAb, and TgAb - are identified and their roles in different thyroid diseases are explained. The document concludes by stating that laboratory testing of thyroid autoantibodies is key for diagnosis of autoimmune thyroid disorders and that treatment often involves inhibiting an overactive thyroid or replacing thyroid hormones.















![ Tortora GJ, Derrickson B. The Endocrine System In: Tortora GJ,
Derrickson B editors. Principles of Anatomy and Physiology
[13th Ed]. John Wiley & Sons; 2011. Pg:696-700.
Pyne D, Isenberg DA. Autoimmune Thyroid Disease in
Systemic Lupus Erythematosus. Annals of the Rheumatic
Diseases. 2001;61:70-72.
Murphy K, Travers P, Walport M. Autoimmunity and
Transplantation In: Murphy K, Travers P, Walportm editors.
Immunobiology [7th Ed]. Garland Science; 2008. Pg:620-21.
Lab Tests Online[Internet]. London: The Association for
Clinical Biochemistry and Laboratory Medicine; c2008 Oct.
Thyroid Autoantibodies; 2008 [cited 2014 July 14]; [about 2
screens]. Available from
http://labtestsonline.org.uk/understanding/analytes/thyroid-
antibodies/tab/sample/
REFERENCES](https://image.slidesharecdn.com/029935d7-adb1-402b-be11-1235173c4279-160723193229/85/Thyroid-autoantibodies-17-320.jpg)