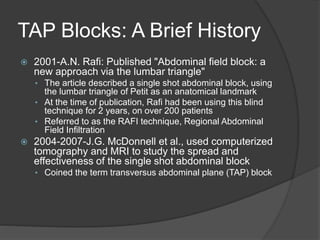
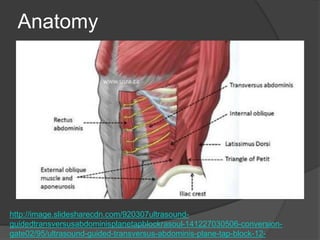
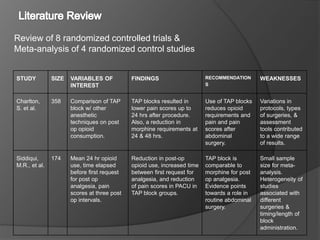
The document summarizes research on transversus abdominis plane (TAP) blocks. It provides a brief history of regional anesthesia techniques leading to the development of TAP blocks. The anatomy of TAP blocks and the technique for administration are described. Several studies are reviewed finding that TAP blocks reduce postoperative opioid consumption and pain scores compared to placebo after various abdominal surgeries. However, the degree of benefit varies across studies. While TAP blocks may decrease pain and opioids, the studies did not find they significantly reduce opioid side effects.