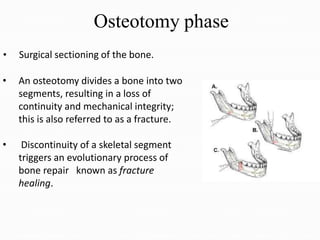
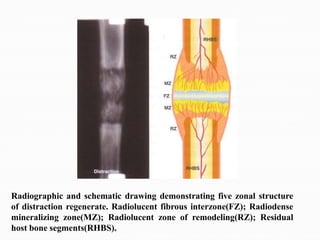
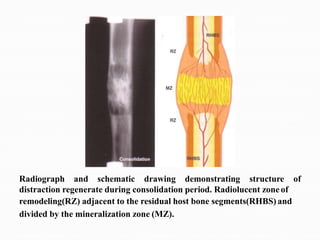
This document provides an overview of distraction osteogenesis. It discusses the history of distraction techniques dating back to the early 1900s. It then covers the indications, contraindications, advantages, and disadvantages of distraction osteogenesis. The document explains the biology and phases of distraction osteogenesis including osteotomy, latency, distraction, consolidation, and remodeling. It discusses variables in the distraction phase such as rate and rhythm. Overall, the document provides a high-level summary of distraction osteogenesis techniques and processes.