The document discusses the approach to hypoglycemia in children, including its definition, symptoms, classification, and emergency management strategies. It highlights the causes of hypoglycemia in infants and children, the importance of diagnosing underlying disorders, and the critical need for timely treatment to prevent long-term neurological damage. The text also includes a case study illustrating the implications of hypoglycemia in a clinical scenario.







![Hormonal Signal:-
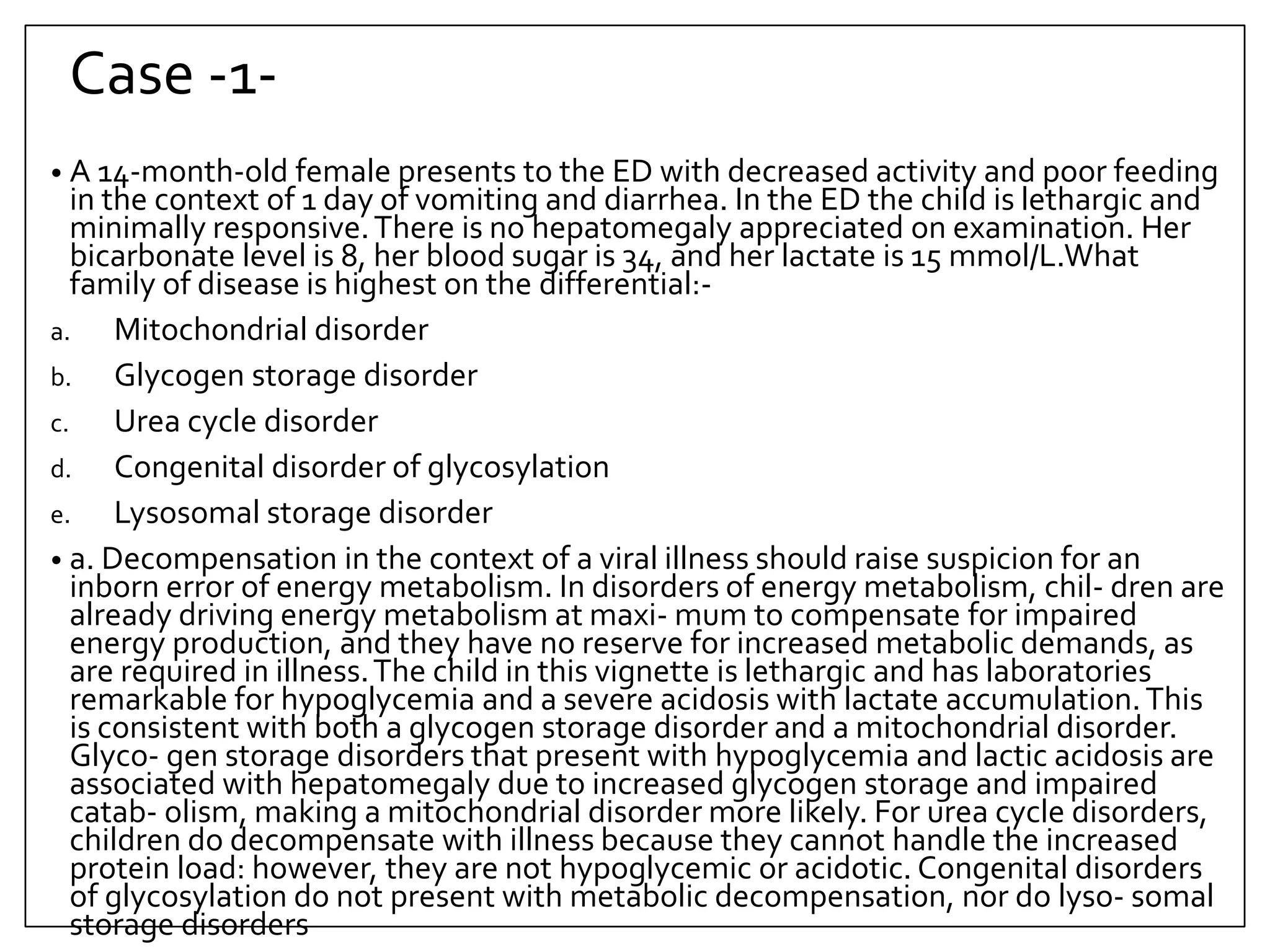
•In a normal individual, a decrease in serum glucose
concentrations leads to:-
▫ Suppression of insulin secretion (to <5 μU/dL)
▫ Increased secretion of the counter-regulatory hormones:-
1. growth hormone [GH],
2. cortisol,
3. Glucagon
4. epinephrine.
8](https://image.slidesharecdn.com/approachtohypoglycemiainchildren-221123213407-b623ac49/75/Approach-to-Hypoglycemia-in-Children-pptx-8-2048.jpg)