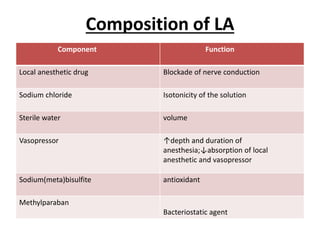
This document provides information on various techniques for local anesthesia in dentistry. It discusses the mechanism of action, classifications, and maximum recommended doses of local anesthetics. It also describes in detail techniques for maxillary injections including inferior alveolar nerve block, Gow Gates, and Vazirani Akinosi techniques for mandibular anesthesia. Complications and contraindications of local anesthesia are mentioned.