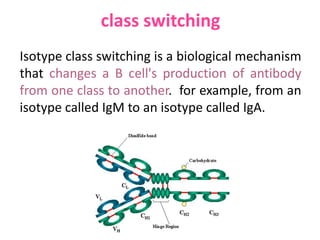
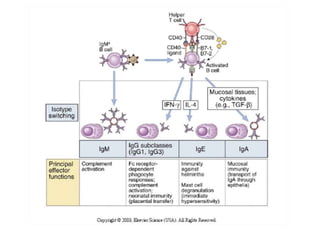
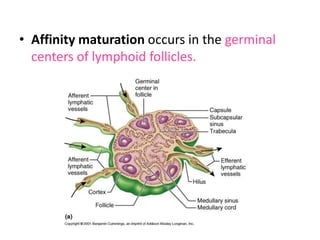
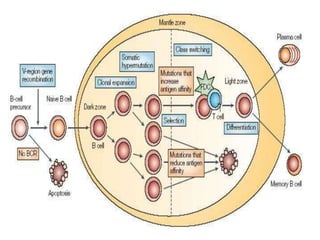
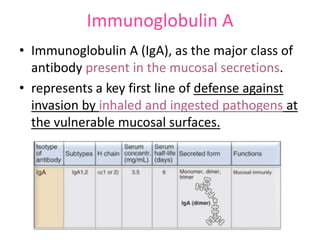
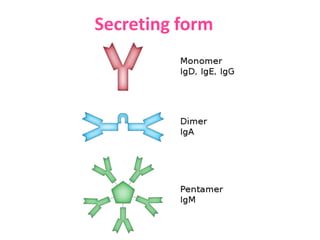
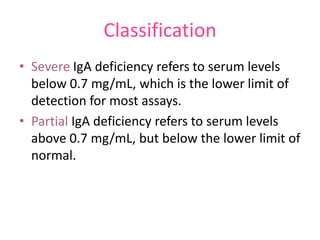
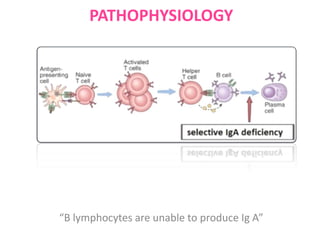
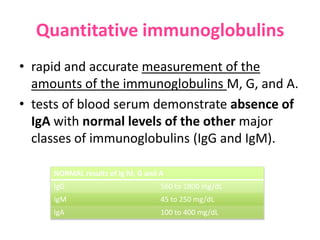
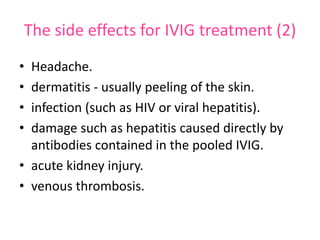
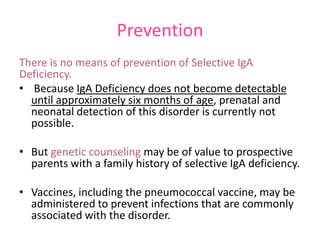
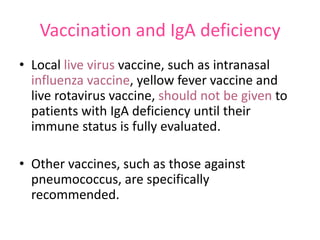
This document discusses selective immunoglobulin A (IgA) deficiency. It begins by defining immunoglobulins, antibodies, and the process of class switching that allows antibodies to change class. It then discusses affinity maturation, where antibodies increase in affinity for antigens over time. Selective IgA deficiency is defined as having low or absent levels of the IgA antibody. Causes may include genetics or unknown factors. Risk is higher in Caucasians. Most people are asymptomatic, but some experience recurrent infections. Diagnosis involves blood tests showing low IgA levels. Treatment focuses on infection management and preventative vaccines. IVIG can treat associated deficiencies.