gait abnormalities in children.ppt
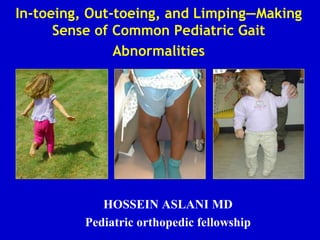
- 1. In-toeing, Out-toeing, and Limping—Making Sense of Common Pediatric Gait Abnormalities HOSSEIN ASLANI MD Pediatric orthopedic fellowship
- 2. Rotational & Angular Deformities in Children Objectives: 1.) Review common physiologic and pathologic causes of in-toeing/out-toeing gait in children 2.) Review diagnosis and physical examination techniques used in assessing pediatric rotational and angular deformities 3.) Review the current management of pediatric rotational and angular deformities in children 4.) Review the differential diagnosis of limping gait/gait abnormality in children
- 3. Rotational & Angular Deformities in Children: Introduction • Rotational and Angular Deformities are quite common in pediatrics • Very diverse spectrum of diagnoses: physiologic to pathologic • In-toeing/Out-toeing, Genu varum (bowlegs)/valgum (knock-knees)
- 4. The In-toeing Toddler or Child • History: Inquire about onset, severity, progression, disability, and previous treatment • Always assess developmental history: when did child start walking independently, gross and fine motor skills • Screening examination to r/o hip dysplasia (DDH), other neurological problems (cerebral palsy)
- 5. Causes of In-toeing Gait in Children • The most frequent causes of childhood in- toeing: Femoral anteversion Medial Tibial Torsion Metatarsus adductus
- 6. The In-Toeing Toddler/Child: Assessment Rotational Profile: Evaluate in four steps 1.) Observe child walking and running. Estimate the foot progression angle (FPA): angular difference between the axis of the foot and the line of progression
- 7. Assessing the Foot Progression Angle • Nonspecific estimation • Normal: usually -5 tp +20 degrees • In-toeing -5 to-10 degrees: mild -10 to -15 degrees moderate >-15 degrees severe
- 8. The In-Toeing Toddler/Child: Assessment 2.) Assess Femoral Version: Measure external and internal rotation of the hips with the child prone and the knees flexed to 90 degrees. Assess both sides simultaneously. Internal rotation usually less than 65-70 degrees If greater than 70 degrees: in-toeing likely from femoral anteversion/femoral torsion If rotation is asymmetrical, evaluate with AP of pelvis to r/o DDH or hip problem
- 9. Assessing Femoral Anteversion: Internal Rotation of the Hip
- 10. Internal Femoral Torsion/Anteversion • In standing position, patellae will point inwards when feet are forward • Compensatory external rotation of tibia
- 11. Femoral Anteversion: Clinical Assessment “Kissing” patellae
- 12. Femoral Anteversion: Definitions • Femoral version defined as the angular difference between axis of femoral neck and the transcondylar axis of knee • Femoral anteversion ranges from 30-40 degrees at birth and decreases progressively to about 10-15 degrees at skeletal maturity • Measurement:X-rays (biplane): technically difficult CT--most accurate method
- 13. Internal Femoral Torsion/Anteversion • Usually first seen in the 3-5 year age group, usually most severe b/w 4-6 years • Almost always symmetrical • Mechanism unknown, genetic factors and position of fetus in uterus causing increased rotation • More common in females: approx. 2: 1 ratio, often familial • Gait/running described as awkward/clumsy by parents
- 14. Femoral Anteversion: Management • Gait is often worse when running or when fatigued • Children prefer the “W” sitting position because it is more comfortable…should not be discouraged or avoided • Reassurance and Observation!! • Special shoes, twister cables, etc avoided….no difference in outcome!!
- 15. Internal Femoral Torsion: Management • Internal femoral torsion/antetorsion • Mild: internal rotation of hip 70-80 degrees • Moderate: internal rotation 80-90 degrees • Severe: internal rotation > 90 degrees • External hip rotation is usually reduced: total arch of rotation is usually 90-100 degrees • Resolves spontaneously without treatment in overwhelming majority of patients: most literature-- 98-99% • Results from decrease in femoral anterversion over time (age 8-9 years) and from a lateral rotation of the tibia
- 16. Femoral Anteversion: Operative Treatment • Indications for Osteotomy: Individualized • Tachdijian indications: femoral anteversion >45 degrees hip unable to laterally rotate beyond neutral, functional disability and severe cosmetic deformity • Must weigh the benefits from procedure versus the morbidity of surgical procedure
- 17. Surgical Treatment of Femoral Anteversion: Derotational Femoral Osteotomy • Because of high spontaneous resolution rate...derotational osteotomy is not done before 8-9 years • Very rare surgery: delayed until adolescence to determine if spontaneous correction will occur
- 18. Internal (Medial) Tibial Torsion • Toddler or young child often presents with c/o “bowing legs” • Usually symmetric in-toeing, if unilateral--usually worse on left • Often noticed when child is first starting to walk • With patellae facing forwards (in neutral position), feet turn in
- 19. Measurement of Thigh Foot Angle: Medial Tibial Torsion 3.) Quantify Tibial Version Thigh Foot Angle: patient is prone, knees flexed 90 degrees: TFA is the angular difference between the axis of the foot and the axis of the thigh • Allow foot to fall into natural position, avoid manual positioning of foot • Medial Tibial Torsion: Negative Thigh Foot Angle
- 20. Internal Tibial Torsion: Diagnosis • Resolves spontaneously in 95-98% of patients by age 4-6 years • Stretching, special shoes are inefffective…does not speed up resolution and makes no clinical difference • Can occasionally have mild persistence with no handicap or functional significance • Usually simple observation is best treatment and all that is needed
- 21. Medial Tibial Torsion: Management • CT Scan is the best diagnostic study to precisely diagnose the degree of torsion • Always pursue conservative treatment: OBSERVATION!! • If medial tibial torsion is causing gait problems and significant disability (usually > 40 degrees internal rotation)... can consider derotational osteotomy after age 8 years (very rare!!)
- 22. Metatarsus Adductus in Infants • Assess the foot for forefoot adductus • Lateral border of foot should be straight • Convexity of lateral border and forefoot adduction are features of metatarsus adductus
- 23. Grading Severity of Forefoot Adductus • Project a line that bisects the heel. Normally it falls on the 2nd toe • Mild: falls through the 3rd toe • Moderate: falls between toes 3-4 • Severe: falls between toes 4-5
- 24. Metarsus Adductus in Infant • Most common foot deformity in children: 1-3/1000 • Prognosis is directly related to the degree of stiffness • Differentiate between metatarsus varus and talipes eqinovarus • Associated with DDH in 2% of cases--careful hip examination
- 25. Metatarsus Adductus: Assessment • Exact cause is unknown • Commonly believed to be caused by intrauterine positioning or crowding • No correlation between gestational age at birth, maternal age, or birth order
- 26. Metatarsus Adductus: Management • Forefoot can gently be stretched passively with each diaper change • Occasionally will use serial casting and reverse/straight last shoes to correct deformity • Observation and Reassurance: will resolve spontaneously in 90-95% of patients (tends to persist until age 12-18 months)
- 27. Physiologic Infantile Out-Toeing • Out-toeing in early infancy is usually due to a lateral rotation contracture of the hips • When infant is positioned upright, the feet will usually turn out • Resolves spontaneously with ambulation…no treatment is needed
- 28. Out-toeing: External Tibial Torsion • Most common cause of out-toeing in children • May worsen over time because of the normal lateral rotation of the tibia that occurs with growth • May be associated with patellofemoral knee pain • If combined with femoral anteversion ( knee internally rotated and ankle externally rotated):“miserable malalignment syndrome”…inefficient gait and patellofemoral joint pain
- 29. Mean Tibio-Femoral Angle In Children
- 30. Lower Extremity Rotational Profile at Various Ages • Normal alignment progresses from 10-15 degrees of varus at birth to maximum valgus angulation of 10-15 degrees at 3-4 years of age
- 31. Genu Valgum (“Knock-Knees): • Physiologic knock-knee deformity very common in children aged 3-5 years • Screening evaluation: normal height and body proportions, symmetrical, localized or generalized, limb lengths equal • Measure rotational profile, measure inter-malleolar distance with the knees together • If generalized deformity, order metabolic screening labs
- 32. Physiologic Genu Valgum: Assessment
- 33. Pathologic Causes of Genu Valgum • Post-traumatic (most common) • Dysplasias • Primary tibial valga • Tumor • Infection • Rickets • Renal osteodystrophy • Congenital deficiency of fibula (fibular hemimelia)
- 34. Post-Traumatic Genu Valgum • Usually results from overgrowth following fracture of the proximal tibial metaphysis in early childhood • May also be due to malunion or soft tissue interposition • Valgus deformity develops during the 1st 12-18 months post-injury due to tibial overgrowth • Management: Most will correct spontaneously over course of years without operative treatment • If deformity persists: osteotomy or hemiepiphyseodesis
- 35. Rickets: Diagnosis and Management • Suspect rickets in child with increasing genu varum/valgum, short stature, poor nutritional status (vitamin D deficiency) • Produces generalized genu varum/valgum with bowing of the diaphysis and distinctive cupping and widening of the epiphysis • Refer to endocrinologist for medical management: Ca, Phos supplementation (Vitamin D resistant form possible) • Correction (if necessary) usually delayed until the end of growth as recurrence of deformity is quite common
- 36. Clinical Assessment: Rickets Costochondral “beading” Severe genu valgum
- 37. Clinical Assessment: Genu Valgum-Rickets Family with Rickets increased varus in toddler, valgus in 5 and 12 year old females
- 38. Genu Valgum: General Management • Age 2-6 years: 95-98% will resolve spontaneously • If intermalleolar distance is > 8-10 cm at age 10 1.) Hemiephiphyseodesis of distal femur and/or proximal tibia 2.) If skeletally mature: a.) tibial varus osteotomy b.) femoral osteotomy: medial closing wedge: if genu valgum > 12-15 degrees and superolateral tilt of joint > 10 degrees
- 40. Physiologic Genu Varum: Assessment • Parents will often note bow leg deformity, usually recognized when child starts to walk (12-18 months) • Commonly bilateral and symmetric bowing • Seldom causes functional disability [X-rays unnecessary until at least 18 months of age] • Physiologic bowing usually spontaneously resolves by the age of two years
- 41. Differentiating physiological Genu Varum vs. Blount’s disease • Physiological: bilateral, symmetrical, metaphyseal- diaphyseal angle <15 degrees, upper tibial metaphysis/ epiphysis normal • Blount’s: unilateral/ bilateral, asymmetrical, metaphyseal- diaphyseal angle > 15 degrees, fragmentation of upper tibial metaphysis, tibial epiphysis slopes medially, norrowing of tibial physis medially, widening laterally Diagnosis of Blount’s cannot be made before age 2 years
- 42. Infantile Blount’s Disease: Radiographs
- 43. Pathological Conditions Causing Varus Deformity of the Legs • Metabolic bone disease: Vitamin D deficiency, Vitamin D refractory rickets • Asymmetrical growth arrest or retardation: Blount’s disease, Trauma, Infection, Tumor • Bone dysplasia: metaphyseal dysplasia • Congenital • Neuromuscular
- 44. Infantile Blount’s Disease: Epidemiology • Risk factors: Obesity, African American,Walking at early age, + Family history • Differential Diagnosis: Physiologic genu varum (metaphyseal-diaphyseal angle less than 15 degrees) Rickets Osteomyelitis, Trauma, Tumor Fibrous dysplasia Metaphyseal chondrodysplasia
- 45. Blount’s Disease: Classification • Infantile: (early onset) onset between 1-3 years, bilateral, usually symmetric, pts often large for age, etiology is abnormal compression on medial proximal tibial physis, may feel bony prominence or “beak” over the medial tibial condyle, often have lateral thrust to gait Very difficult to differentiate from physiologic varus/ bowlegs in patients < 2 years Adolescent: (onset over 11 years) often presents with tenderness/pain over the medial prominence of the proximal tibia, pts often obese Prevalence: General population <0.3%, Obese African American male:2.5%
- 46. Metaphyseal/Diaphyseal Varus Angle • Often used to differntiate physiologic from Blount’s disease • If greater than 15-17 degrees, tibia vara or Blount’s disease is likely • Follow radiographs every six months….physiologic varus will gradually improve after age 2 years while Blount’s will progressively worsen
- 47. Measuring the Tibial-Femoral Angle • Line is drawn down center of tibia and femur…. Intersecting angle is the tibio-femoral angle
- 49. Adolescent Blount’s Disease • Definition: Growth disorder involving the medial portion of the proximal tibial growth plate that produces a localized varus deformity • More often unilateral, usually seen in obese individuals, slightly more males than females, African American, certain geographic regions • Definite cause unknown: biomechanical overload to proximal tibia physis due to varus alignment and excessive body weight
- 50. Adolescent Blount’s: Theorized Cause of Progressive Varus Deformity Childhood Varus Rapid Weight Gain Medial Growth Plate Injury Progressive Varus Knee
- 51. Adolescent Blount’s Disease: Clinical Assessment
- 52. AP Radiographs: Assessing the Tibia Vara Deformity Right 30 Left 26
- 53. Blount’s Disease: Non-Operative Treatment • Non-operative: Observation only until age 2 years • Anti-Blount’s Brace: Usually used for pts aged 2-3 years with: 1.) metaphyseal/diaphyseal angle > 15-17 degrees 2.) tibial/femoral angle > 15 degrees 3.) brace is designed to provide rotational support, usually worn FT 4.) usually takes 1 year to determine effectiveness of brace 5.) brace is ineffective in adolescents • If operative correction necessary in infantile Blount’s….results are better when done before the age of 4 years
- 54. Blount’s Disease: Operative Treatment • For optimum correction and results in infantile tibia vara: Surgical treatment in early stages is crucial Avoids sequelae of joint incongruity, limb shortening, and persistent angulation • Proximal tibial osteotomy: distal to patellar tendon insertion (avoid proximal physis (dome, closing or opening wedge) • Adolescent tibia vara: predominately surgical treatment: 1.) Lateral epiphyseodesis: recommended as initial procedure if more than one year of growth remaining 2.) High tibial osteotomy with internal fixation ( usually correct to about 0-5 degrees of varus) 3.) Realignment by external fixation: Ilizarov, Dynamic Axial External fixator, Taylor Spatial Frame
- 55. Surgical Correction: Proximal Tibial Osteotomy • Demonstration of opening wedge tibial osteotomy procedure for correction of infantile blount’s disease • Usually recommend slight overcorrection into mild valgus (reverse excessive compression forces medially: avoid injury to physis)
- 56. Adolescent Blount’s: Realignment by External Fixation-Taylor Frame
- 57. Rotational and Angular deformities: Summary • Most rotational/alignment problems are physiological and will resolve without intervention • Good history and physical examination important • Investigate more if asymmetrical, rapidly progressive • Orthotics, special braces/shoes, twister cables are frequently not helpful or necessary • Most will never require surgery
- 58. The Limping Child…. • Relatively large differential diagnosis list • Obtain good history: VERY important • Observe child…do they look sick, do they have fever, will he/she put weight on leg or let you move extremity?---rule out septic arthritis/infection first!! • Determine history of trauma, fall, or injury? • Age of patient, duration of symptoms, onset of symptoms, family history
- 59. The Limping Child • Observe Child walking/running in hallway • Generally 4 types of limping gait described 1.) Antalgic gait: shortened stance 2.) Abductor lurch: trendelenburg gait 3.) Equinus gait: toe toe progression 4.) Circumduction gait: leg length discrepency
- 60. Limping Gait in Child: Differential • Fracture, Trauma, Overuse: MOST common • Transient synovitis: Must differentiate from septic arthritis • Discoid Lateral Meniscus • Infection: septic arthritis, lyme disease, osteomyelitis • LCPD, SCFE, DDH: Hip pathology • Cerebral Palsy, Neurologic disorders • Neoplasm/Tumor: benign, malignant • JRA, other Rheum disorders The cause of a limp can range from a life-threatening bone tumor to a pebble in a shoe!
- 61. The Limping Child: Transient Synovitis vs Septic Arthritis Transient synovitis •Child refuses to walk •Movement of hip is painful •May have fever •Moderately elevated WBC •Lasts a few days •Disappears without treatment
- 62. Bacteria Enzymes Destroy cartilage Irreversable joint damage White cells Enzymes The Limping Child: Septic Arthritis
- 63. The Worst Scenario…. • Destruction of articular cartilage • Destruction of femoral head • Destruction of femoral neck Septic Arthritis of the Hip
- 64. Treatment: 1. Kill the bacteria! • IV Antibiotics 2. Eliminate the white cells • Early Incision and drainage 3. Don’t delay!!! The Limping Child: Septic Arthritis
- 65. • How to tell the difference? • Four predictors – History of fever >101.5 – Refusal to weight-bear – ESR > 40 mm/hr – WBC > 12,000 • If in doubt… – Review in 12 hours – Do incision and drainage! The Limping Child: Transient Synovitis vs. Septic Arthritis