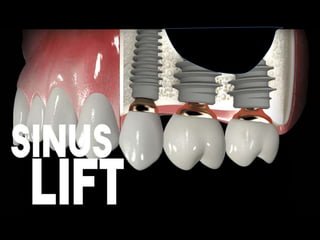
sinus lift
- 2. OUTLINE • INTRODUCTION • ANATOMY OF MAXILLARY SINUS • ARMAMENTARIUM • DECISION TREE • LATERAL WINDOW – WITH GRAFTING – WITHOUT GRAFTING • TRANSALVEOLAR – WITH GRAFTING – WITHOUT GRAFTING • ADVANCED SURGICAL TECHNIQUES – BALLOON LIFT – HYDRAULIC PUMP
- 3. INTRODUCTION • Placement of implants in maxilla is frequently compromised or impossible due to – Atrophy of the alveolar process, – Poor bone quality, – Maxillary sinus pneumatization. • Treatment of choice is influenced by – The vertical height of the residual alveolar bone, – Local intrasinus anatomy – Number of teeth to be replaced
- 5. ANATOMY OF THE MAXILLARY SINUS
- 6. • Largest of the four bilateral air-filled cavities in the skull. • Located in the body of maxilla 34*33*23mm • Pyramidal-shaped structure having as its base the medial wall (the lateral nasal wall). • The pyramid has three main processes or projections: – (1) the alveolar process inferiorly (bounded by the alveolar ridge), – (2) the zygomatic recess (bounded by the zygomatic bone), and – (3) the infraorbital process pointing superiorly (bounded by the bony floor of the orbit, and below it, the canine fossa). • The alveolar and palatine processes form the floor, which after the age of 16 usually lies 1–1.2 cm below the floor of the nasal cavity. • Occasionally it may be divided into two or three compartments by bony septa. • The four sinus cavities are all lined with pseudostratified, ciliated, columnar epithelium overlying a layer of periosteum in contact with the bony sinus walls. • bilaminar structure (schneiderian membrane) and its inner specialized epithelial lining is contiguous with the lining of the nasal cavity through an opening known as the natural ostium.
- 9. NERVES AND BLOOD VESSELS • Sensory innervation of the maxillary sinus is supplied by the maxillary division on the trigeminal nerve (V-2) and its branches. • The posterior superior alveolar nerve, anterior superior alveolar nerve, infraorbital nerve, and greater palatine nerve. The middle superior alveolar nerve contributes to secondary mucosal innervation. • The blood supply to the maxillary sinus is supplied by branches of the internal maxillary artery. • The infraorbital artery runs with the infraorbital nerve in the floor of the orbit, • The lateral branches of the sphenopalatine and greater palatine arteries, and in the floor of the sinus, the posterior, middle, and anterior superior alveolar arteries. • Venous drainage runs anteriorly into the facial vein and posteriorly into the maxillary vein, jugular vein, and dural sinus system.
- 10. FUNCTION OF THE MAXILLARY SINUS • Humidifying and warming inspired air. • Regulation of intranasal pressure. • Increasing surface area for olfaction. • Lightening of the skull mass. • Resonance. • Absorbing shock, helping to lessen brain trauma. • Contributing to facial growth. • Mucociliary propulsion of mucous and serous secretions toward the ostium.
- 11. ARMAMENTARIUM
- 15. DECISION TREE FOR MAXILLARY SINUS ELEVATION OPTIONS
- 16. DECISION TREE FOR MAXILLARY SINUS ELEVATION OPTIONS Fugazzotto PA. Augmentation of the posterior maxilla: a proposed hierarchy of treatment selection. J Periodontol 74 (2003):1682–1691. Chiapasco M, Zaniboni M, Rimondini L. dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res 19 (2008):416–428.
- 17. Fugazzotto PA. Augmentation of the posterior maxilla: a proposed hierarchy of treatment selection. J Periodontol 74 (2003):1682–1691. Chiapasco M, Zaniboni M, Rimondini L. dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res 19 (2008):416–428.
- 20. INCISION (FLAP DESIGN) • A bevel horizontal incision (at 1–2 mm palatal to the alveolar crest and at least 4–6 mm away from the estimated border of the hard tissue outline “window”) • Buccal vertical releasing incisions are placed at the mesial and distal extension of the horizontal incision. • Full-thickness buccal flap is reflected from the crestal side all the way to 4–6 mm apically beyond the upper portion of the bony window outline. • Tip: 4–6 mm clearance provides a safe zone for suture materials. (the suture line will lie on the solid native bone, not the graft materials.
- 21. OUTLINE OF THE BONY WINDOW • Window outline is prepared - lateral aspect of the buccal alveolus. • Size of the window is determined by the area to be grafted in the lateral aspect of the buccal alveolus. • Osteotomy (window) can be oval or rectangular. • Inferior hard tissue outline of the window 3–5 mm above the sinus floor. • Size of the upper window - determined by length of the implant. • Mesial border can be extended as far as distal to canine, and the distal border - tuberosity - mesio- distal implant placement. A carbide bur is only used in thick buccal wall for initial preparation; then switch to a diamond bur/piezosurgical insert.
- 22. PREPARATION OF THE BONY WINDOW • High speed - advantage of saving time but is more technically sensitive. • No. 4, 6, or 8 diamond round bur with copious saline irrigation is utilized to outline window • the osteotomy is deepened in smooth, light sweeping motions until the bone is thin and translucent enough to visualize the underlying gray/red color of the sinus membrane
- 23. HANDLE THE BONE ISLAND • Techniques - handle “remaining bone island” • Tatum - infracture of the bone island and carefully elevating the sinus membrane so that the bone island will lie on top of the graft materials and form the roof of the sinus grafts • Wall-off technique involves removing the bony island completely from the surrounding wall with sinus lift elevators.
- 25. ELEVATE THE SINUS MEMBRANE • Gently detach the membrane at the apical aspect of the sinus cavity and then the mesial and distal aspects. • After initially releasing the lower border, mesial, distal aspect, and upper border of the sinus membrane about 3–5 mm, • Go farther from the lower aspect of the sinus cavity to separate all the way to the medial wall. • It is important to ensure that the membrane is lifted high enough to place the appropriate implant length
- 28. BONY WINDOW OSTEOTOMY • Sinus lift kit includes inserts: OT1, OT5, EL1, EL2, and EL3. • Reduction of the thickness of the lateral sinus wall until the dark shadow. • Indicating sinus cavity is seen - achieved by using osteoplasty insert (OP5 or OT5) from Mectron system. • Once the thickness of the wall is reduced to 1 mm or less, the window is outlined by either sinus bony window osteotomy insert (OT1: diamond scalpel insert) or by OT5 (round diamond insert). • Ideal shape of the window is oval and the length of the window depends on the number and location of implants. • Window preparation can be completed by OT1 or OT5 inserts.
- 29. SINUS MEMBRANE SEPARATION • Sinus membrane separator (EL1) insert (compressor) is inserted into the frame of the window and is used to separate the Schneiderian membrane. • With the help of cavitation, this insert can start elevating the membrane internally (for up to 2 mm around the margins of the window). • Separation reduces membrane tension and results in membrane mobility, and at this point the membrane can be manually lifted
- 30. SINUS MEMBRANE ELEVATION BY NON CUTTING ELEVATOR EL1, EL2, AND EL3 • Sinus membrane elevators (EL2 and EL3 are both non cutting elevators) help further separation in internal zones of the window
- 31. BONE GRAFT MATERIALS AND BARRIER MEMBRANE • (1) incorporate xenografts for a slower resorption rate compared with allografts (DFDBA/FDBA); • (2) use xenografts or alloplasts if space maintenance of the matrix materials in the sinus is desired; and • (3) possibly add to the matrix materials biologics if one desires enhancement of the quality of the bone formed in a shorter time period. • A recent study has shown the addition of rhBMP-2/ACS to bio-Oss has a negative effect on bone formation • Tight compaction of the graft material - decreased bone formation (decrease in space between the particles and a decrease in bone formation between the particles). Kao dW, Kubota A, Nevins M, Fiorellini JP. the negative effect of combining rhbMP-2 and bio-Oss on bone formation for maxillary sinus augmentation. Int J Periodontics Restorative Dent 32 (2012):61–67.
- 33. THE LATERAL WINDOW TECHNIQUE WITH A GRAFTING MATERIAL AND SIMULTANEOUS OR DELAYED IMPLANT INSTALLATION • Tatum (mid-70s) afterwards described by boyne and james in 1980 • The maxillary sinus is exposed through oral mucosa in region of anterior, lateral maxillary sinus wall. • A midcrestal incision is made with posterior and anterior vertical releasing incisions. • A mucoperiosteal flap with trapezoid base - reflected exposing lateral wall of sinus. • A trapdoor osteotomy is performed on the lateral wall of sinus with burs or piezoelectric surgery avoiding laceration of the schneiderian membrane. • The trapdoor is infractured, schneiderian membrane is carefully dissected, elevated from the floor, lateral, medial sinus wall. • Displaced dorsocranially with blunt dissector to create a compartment for placement of the graft.
- 35. • Implant placement simultaneously, if the height of the residual alveolar bone provides sufficient primary stability. • An implant bed is successively prepared with burs, implant tip exposed in the created compartment in the maxillary sinus. • The graft material is densely packed around the exposed implant surface to facilitate de novo bone formation • The lateral window covered by a resorbable collagen membrane to prevent ingrowth of fibrous tissue before the mucoperiosteum is readapted and sutured. • If stability is compromised, then the implants are inserted 4 to 12 months after the augmentation. • Final prosthetic solution is performed three to six months after implant installation.
- 36. • The implant survival rate was equivalent regardless of the used graft material and time of implant placement . • Metaanalysis, long-term implant treatment outcome concluded that maxillary sinus floor augmentation with autogenous bone graft, mixture or bone substitutes alone - highly predictable and successful enhance the vertical alveolar bone height before or in conjunction with implant placement. Starch-Jensen T, Aludden H, Hallman M, Dahlin C, Christensen AE, Mordenfeld A. A systematic review and metaanalysis of long-term studies (five or more years) assessing maxillary sinus floor augmentation. Int J Oral Maxillofac Surg. 2017 May 22. [Medline: 28545806] [doi: 10.1016/j.ijom.2017.05.001] . Ting M, Rice JG, Braid SM, Lee CYS, Suzuki JB. Maxillary Sinus Augmentation for Dental Implant Rehabilitation of the Edentulous Ridge: A Comprehensive Overview of Systematic Reviews. Implant Dent. 2017 Jun;26(3):438-64.
- 37. RADIOLOGICALAND HISTOMORPHOMETRIC OUTCOME • Systematic reviews histomorphometric autogenous bone graft resulted in the highest amount of newly formed bone comparison to various bone substitutes - Corbella s 2016. • Higher proportion of mineralized bone during the early healing phase • A healing period of more than 9 months no significant differences - Corbella s 2016. • Effect of a barrier membrane similar bone formation with or without - Suárez-lópez del amo f 2015. • No evidenced beneficial effect of platelet concentrates due to large heterogeneity among the included studies - Del fabbro 2013. • Bone-to-implant contact was significantly higher when autogenous bone graft or DBBM as compared to DBBM alone, after 12 weeks - Jensen T 2013. • Fluorochrome labelling - early bone to implant contact formation adjacent to the implant surface was more advanced with autogenous bone graft compared to DBBM - Jensen T 2013. • Some loss of the augmentation volume always occurs, but bone substitutes or composite grafts display less volume reduction compared to autogenous - Shanbhag S 2014
- 38. COMPLICATIONS • Perforation of the Schneiderian membrane is the most common. • Presence of sinus septa and a residual bone height less than 3.5 mm increases the risk for a sinus membrane perforation - Schwarz L 2015. • However, perforation of the Schneiderian membrane seems not to influence the final treatment outcome. • but a higher prevalence for sinusitis is reported in cases of membrane perforation - Schwarz L 2015 • Other complications include bleeding, migration of dental implants into the maxillary sinus, postoperative infection, sinusitis, exposure of the graft, graft loss, oedema, seroma formation, benign paroxysmal positional vertigo and exposure of the collagen membrane. • smoking seems to be associated with increased risk of wound dehiscence and infection - Schwarz L 2015 Schwarz L, Schiebel V, Hof M, Ulm C, Watzek G, Pommer B. Risk Factors of Membrane Perforation and Postoperative Complications in Sinus Floor Elevation Surgery: Review of 407 Augmentation Procedures. J Oral Maxillofac Surg. 2015 Jul;73(7):1275-82.
- 39. CONCLUSION AND CLINICAL RECOMMENDATION • Safe and predictable surgical procedure with low morbidity. • When the height of the residual alveolar bone is less than 6 mm.
- 40. LATERAL WINDOW TECHNIQUE WITHOUT A GRAFT MATERIALAND SIMULTANEOUS IMPLANT INSTALLATION • Introduced by Lundgren et al 2004. • Requires sufficient vertical height achieve primary implant stability, since immediate implant installation is necessary to preserve and support the elevated schneiderian membrane • Allowing coagulum formation round the exposed implant surface in the sinus cavity. • Short-term non-comparative studies - Silva LD 2016, but long-term studies are scarce.
- 41. SURGICAL TECHNIQUE • Similar - usually prepared with an undersized drilling protocol. • A blood coagulum is formed around the exposed implant tip in the secluded compartment between the elevated and the original floor • The lateral window to the maxillary sinus is covered by a resorbable collagen membrane. • The mucoperiosteum is readapted and sutured • Final prosthesis - performed three to six months after elevation and implant installation, when de novo bone is formed around the implant.
- 43. CLINICAL OUTCOME • Implant survival rate beyond 90% - Silva LD 2016. • Longterm studies are scarce. • Moreover, an implant survival of 99% has been described in a 1 to 6-year follow-up study - Cricchio G, 2011. • However, only 14 implants inserted in 6 patients were followed for 6 years - Cricchio G, 2011. Cricchio G, Sennerby L, Lundgren S. Sinus bone formation and implant survival after sinus membrane elevation and implant placement: a 1- to 6-year follow-up study. Clin Oral Implants Res. 2011 Oct;22(10):1200-12.
- 44. RADIOLOGICALAND HISTOMORPHOMETRIC OUTCOME • Average vertical alveolar bone gain after 6 months was 7.9 mm without a graft material and 8.3 mm when an autogenous bone graft. Borges FL 2011 • Radiographic assessment - bone density was significantly higher in sinuses augmented with a blood clot compared to an allogenic graft after 6 months. Altintas NY 2013. • Intra-sinus vertical height increased significantly for implants protruding longer into the sinus cavity compared to implants with only a minor part of the implant tip exposed. • Histologic evaluation - revealed new bone formation, mean vital bone volume varying 39% and 60%, after 6 months. Altintas NY, Senel FC, Kayıpmaz S, Taskesen F, Pampu AA. Comparative radiologic analyses of newly formed bone after maxillary sinus augmentation with and without bone grafting. J Oral Maxillofac Surg. 2013 Sep;71(9):1520 Falah M, Sohn DS, Srouji S. Graftless sinus augmentation with simultaneous dental implant placement: clinical results and biological perspectives. Int J Oral Maxillofac Surg. 2016 Sep;45(9):1147-53.
- 45. COMPLICATIONS • A higher risk of sinus membrane perforation has been reported, when the lateral cortical bony window was dissected free and removed from the underlying schneiderian membrane - Cricchio G 2011 • Implant loss has been reported in a case with a perforation of the sinus membrane. • Postoperative infection. • Exposure of the covering membrane, • Swelling, • Mild postoperative oedema, • Pain, • Loosening of healing abutments, • Nose bleeding Cricchio G, Sennerby L, Lundgren S. Sinus bone formation and implant survival after sinus membrane elevation and implant placement: a 1- to 6-year follow-up study. Clin Oral Implants Res. 2011 Oct;22(10):1200-12.
- 46. CONCLUSION AND CLINICAL RECOMMENDATIONS • Safe and predictable surgical procedure with few complications and a high short- term implant survival rate. • However, no consensus has yet been reached on the amount of bone formation and predictability. • long-term are scarce. • should solely be recommended for single implant installation, when a limited amount of bone regeneration is needed - Starch-Jensen 2017
- 48. OSTEOTOME-MEDIATED ELEVATION AND SIMULTANEOUS INSTALLATION OF IMPLANTS WITH OR WITHOUT THE USE OF A GRAFT MATERIAL • Transcrestal sinus lift approach -Tatum in 1986. • 1994 Summers - set of tapered osteotomes with increasing diameters intended to increase the density of the soft bone and create an up-fracture of the maxillary sinus floor. • Schneiderian membrane and the maxillary sinus floor is elevated from a transcrestal approach using osteotomes creating a compartment for graft placement and/ or blood clot formation, without the preparation of a lateral window. • Implants are inserted immediately to support the elevated floor of the maxillary sinus with the Schneiderian membrane. • Most suitable for installation of a single implant, can be used for multiple implants. • Less invasive and time-consuming.
- 49. CLINICAL PROCEDURES OF THE TRANSALVEOLAR OSTEOTOME • Using a 2 mm cylindrical bur, the implant site - prepared depth 1 mm below the sinus floor - safety zone, prevent tip of drill from rupturing membrane • A periapical radiograph is taken with the 2 mm guide pin in place - confirm integrity of the subsinus cortex, verify implant position and distance from apex of osteotomy to floor • osteotomy enlarged 3 mm cylindrical drill to the desired depth, which should remain 1 mm below the sinus floor • before any attempts to elevate, graft material is added to the osteotomy. the volume of material should not exceed 2–3 mm in height - inadvertent perforation of the sinus membrane less likely • A 3 mm osteotome is inserted into the osteotomy and advanced with light malleting • it is difficult to quantify the tapping force because the remaining bone quality and quantity differ between cases. • However, if you feel a high degree of resistance or the osteotome does not advance, you may use a small diameter round bur or piezosurgical instruments to delicately pierce a dense spot of apical bone. • Once the osteotome is advanced to the depth of the sinus floor, infracturing the cortical bone, the remaining bone is pushed apically into the sinus cavity, • elevating the sinus membrane. the instrument can then progress about 2 mm deeper than the depth of the infracture at each time. bone graft material must be added into the osteotomy at each advancement. • At no point should the tip of the osteotome penetrate into the sinus or touch the Schneiderian membrane. • Once the tip of the osteotome has reached the desired height, the osteotomy is widened with a larger diameter osteotome, such as 3.5 mm. the sequence of adding graft material and tapping the osteotome to the predetermined depth continues until the necessary amount of elevation is achieved • the final osteotome diameter should be narrower than the desired implant width, typically 0.5–1.2 mm less.
- 50. • Undersizing the osteotomy will allow osteocompression during implant placement, especially in type IV bone. • For example, the final osteotome for a 4 mm implant would be 3.5 mm, and for a 5 mm implant, a 4.2 mm would be final osteotome • the final step of the osteotome procedure is to test the resistance by inserting the final osteotome or guide pin to the desired length. • Additional graft material should be added to the osteotomy prior to implant placement. the actual insertion of the implant will displace the material more apical and lateral, stretching the Schneiderian membrane even further. it is recommended that 2–3 mm of bone graft material around the apex of the implant may add the implant primary stability . • the osteotome approach can be also combined with extraction.
- 55. • It is recommended that there be 2 mm of graft material around the apex of the implant after osteotome procedures. • The original summers osteotomes are continous taper and concave tips. The concave design can collect and hold the bone and also assist in pushing bone graft materials in front of the advancing osteotome. • Osteotomes typically have a concave tip that serves to cut and collect bone. This allows for the vertical compression of the bone. It is the apical displacement of the bone that is collected by the osteotome that will cause elevation of the sinus floor and schneiderian membrane. • A surgical mallet is used to advance the osteotome. • The surgeon may identify the cortical floor of the sinus cavity by the change in tactile sensitivity while malleting the osteotome. • A different pitch of tapping the osteotomes are available as straight instruments as well as offset to allow access in the more posterior areas or when there is limitation of opening. The magnitude of apical force and tactile sensitivity may be diminished with use of the offset osteotomes. • There are also osteotomes with convex tips. The convexity will create horizontal compression. When convex tips are used, they are alternated with concave tips to achieve both vertical and horizontal compression. • Polyflouroethylene (gore-tex), a nonresorbable suture, in these procedures allows the wound to heal properly and without separation of the incision line.
- 60. CLINICAL OUTCOME • Overall implant survival rate higher than 90% - Shi JY 2016 • No statistically significant difference with or without the use of a graft material - Chen MH 2017 • A 10-year implant survival rate of 100% without the use of a graft material [62]. • The implant survival rate - higher when the residual vertical alveolar bone height is more than 5 mm - Del Fabbro M 2012 • Installation of short implants (≤ 6 mm) in conjunction with osteotome-mediated sinus floor elevation significantly diminished the implant survival rate - Lang NP 2000
- 61. RADIOLOGICALAND HISTOMORPHOMETRIC OUTCOME • Significantly more bone gain with a grafting material compared to the use of no graft. • 10-year intra-sinus new bone formation was 3 mm without the use of a graft material. • Bone formation was more pronounced during first year and tends to increase for three years. • Osteotome-mediated sinus floor elevation with a graft material and simultaneous installation of implants seem to facilitate more vertical alveolar bone gain compared to the use of no graft material Pjetursson BE, Ignjatovic D, Matuliene G, Brägger U, Schmidlin K, Lang NP. Maxillary sinus floor elevation using the osteome technique with or without grafting material. Part II – Radiographic tissue remodeling. Clin Oral Implants Res. 2009 Jul:20(7):677-83
- 62. COMPLICATIONS • Perforation of the Schneiderian membrane with a mean incidence of 3.8%. • An oblique maxillary sinus floor, sinus septa and root apices penetrating into the maxillary sinus increases the risk. • Not influence the implant survival rate. • Postoperative infection, disorientated after surgery, nose bleeding, blocked nose, hematomas, benign paroxysmal positional vertigo and postoperative bleeding. Tan WC, Lang NP, Zwahlen M, Pjetursson BE. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part II: transalveolar technique. J Clin Periodontol. 2008 Sep:35(8 Suppl): 241-54
- 63. CONCLUSION AND CLINICAL RECOMMENDATIONS • Predictable and reliable approach with a high implant survival rate. • Installation of short implants (≤ 6 mm) significantly diminished the implant survival rate. • Indicated when a residual vertical alveolar bone height of more than 6 mm is present. • Autogenous bone graft or bone substitutes can be added, if more intra-sinus bone gain is needed for installation of implants with a desirable length.
- 65. SINUS LIFT BALLOON • The zimmer inflated sinus balloon was designed to lift the schneiderian membrane gently and uniformly. • The balloon instrument can also be used to anticipate the required bone graft material, such as 1 cc of saline, which is used to inflate the balloon, equal to 1 cc of grafting material. • On average, with 1 cc of saline the sinus lift balloon may elevate sinus membrane 6 mm. • Angled design can be used in the lateral window/caldwell-luc approach. • Straight design can be used in the crestal/summers approach • Micro-mini design can be also used in the crestal/summers approach with a small diameter opening (1.9 mm)
- 66. Sotirakis EG, Gonshor A. Elevation of the maxillary sinus floor with hydraulic pressure. J Oral Implantol 31 (2005):197–204.
- 67. CLINICAL PROCEDURES • Step 1 (to create access) the initial osteotomy (a pilot drill of 2 mm in diameter) is performed to a depth approaching the floor stopping 1–2 mm short of the floor. • A small diameter osteotome can be used to penetrate the sinus floor • A guide pin is used to indicate the depth of the osteotomy. • Step 2 (to insert the sinus lift balloon) it is recommended to inflate and deflate the balloon extraorally several times with saline before inserting into the sinus cavity • Make sure not to overinsert the metal tube into the sinus cavity - membrane tear. • Step 3 (to detach the sinus membrane) once the balloon is inserted into the sinus cavity, the balloon can be pumped with normal saline. • On average with 1 cc of saline the sinus lift balloon may elevate the sinus membrane 6 mm. • Step 4 (bone grafting material placement) The dome-shaped bone grafting material can be seen via radiograph. • Step 5 (dental implant placement)
- 69. HYDRAULIC SINUS LIFT • to minimize the tapping motion by using hydraulic pressure, “hydraulic sinus lift”. • the unregulated hydraulic pressure is applied into the osteotomy site by means of air/water exhaust spray from handpiece or an uncontrolled water jet to detach the Schneiderian membrane -loosen the membrane. • Without controlling the direction and intensity distribution of the hydraulic pressure, sinus membrane perforations may still occur, pressure is directed against the apex of the “tent” being created. • to provide suitable equal distribution of hydrostatic pressure, “controlled hydrostatic sinus elevation” was introduced - “lifting pressure” that simultaneously places equal force per square millimeter of bone-membrane interface. • Hydraulic pressure in a closed system places equal pressure on all surfaces within the system, thereby eliminating “point sources” of pressure, and gently elevating membrane equally at all points of attachment. - a calibrated, hand-controlled pump and pressure sensormeter.
- 71. SURGICAL PROTOCOL • Surgical step 1 (to create access) the initial osteotomy (a pilot drill of 2 mm in diameter) ,depth approaching the floor of the sinus cavity but stopping 1–2 mm short of the floor. • A diamond piezosurgical drill can also be used to just gently perforate the floor of the sinus bone without harming the membrane. • the piezeoelectric device is designed to cut or grind bone but not damage adjacent soft tissue. • the integrity of the sinus membrane is then examined by Valsalva maneuver or direct visualization. Chen L, Cha J. An 8-year retrospective study: 1,100 patients receiving 1,557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol 76 (2005):482–491.
- 72. • Step 2 (initial detachment of the sinus membrane)- after clearing all the air from the tubing, the Luer-Lock cannula with tapered plug-in end (2 mm diameter) is inserted into the osteotomy preparation before touching the sinus floor and pressed snugly using finger pressure. • the normal isotonic saline fluid is pumped slowly into the closed system, and the gentle pressure will begin to elevate the membrane via the hydrostatic pressure from the hand-actuated pump. • the pressure sensor meter inserted into the closed system will monitor the pressure and also indicate the force necessary to just detach membrane without tearing. • it is imperative that the bone- to-cannula interface be airtight so that there is no lateral leakage of the normal saline solution. • Step 3 a second examination of the integrity of the sinus membrane is done. • After the initial lift is complete, the surgeon switches to a 3 mm implant drill through the previous osteotomy site. • then, the previous controlled hydrostatic sinus lift procedure is repeated - matched larger-sized cannula and tools. the sinus membrane is now lifted to the desired extent, followed by placement of bone graft.
- 73. REFERENCES • Anitua E, Prado R, Orive G. A lateral approach for sinus elevation using PRGF technology. Clin Implant Dent Relat Res 11 (2009):e23–31. • bornstein M, Chappuis V, Von Arx t, buser d. Performance of dental implants after staged sinus floor elevation (SFE) procedures: 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res 19 (2008):1034–1043. • deporter dA, Caudry S, Kermalli J, Adegbembo A. Further data on the predictability of the indirect sinus elevation procedure used with short, sintered, porous-surfaced dental implants. Int J Periodontics Restor Dent 25 (2005):585–593. • Hallman M, Sennerby L, Lundgren S. A clinical and histologic evaluation of implant integration in the posterior maxilla after sinus floor augmentation with autogenous bone, bovine hydroxyapatite, or a 20:80 mixture. Int J Oral Maxillofac Implants 17 (2002):635–643. • Kim yK, Kim SG, Park Jy, yi yJ, bae JH. Comparison of clinical outcomes of sinus bone graft with simultaneous implant placement: 4-month and 6-month final prosthetic loading. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111(2011):164–169. • Zinner id, Small SA. Sinus-lift graft: using the maxillary sinuses to support implants. JADA 127 (1996):51–57. • Zitzmann NU, Schärer P. Sinus elevation procedures in the resorbed posterior maxilla: comparison of the crestal and lateral approaches. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85 (1998):8–17.