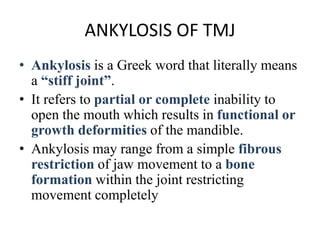
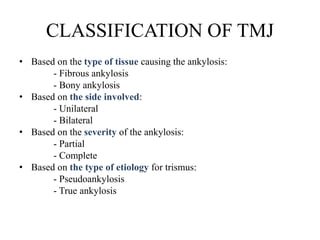
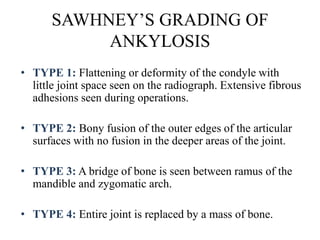
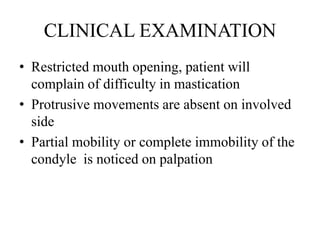
- Ankylosis is a stiffening of the temporomandibular joint (TMJ) that results in restricted opening of the mouth. It can range from fibrous restrictions to complete bony fusion of the joint.
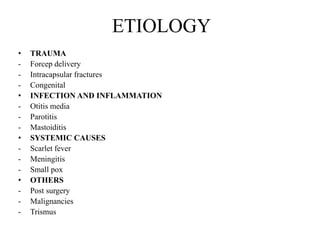
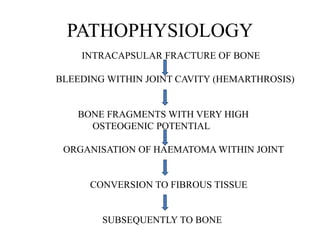
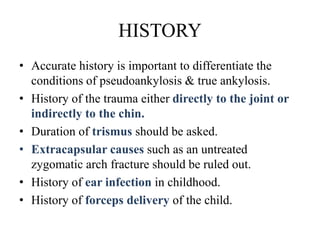
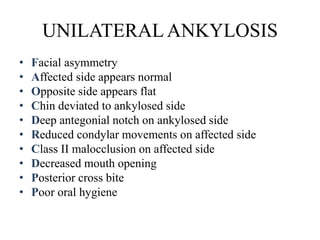
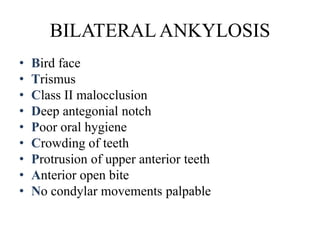
- Common causes include trauma, infection, and systemic diseases. Intra-articular fractures lead to bleeding in the joint cavity and bone fragments with high osteogenic potential can fuse the joint.
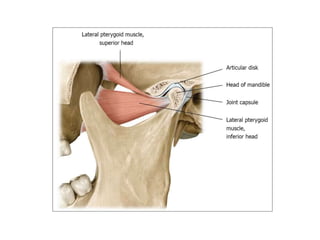
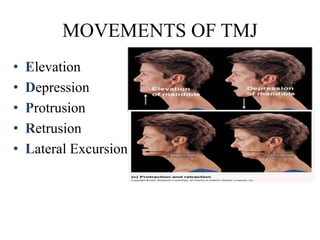
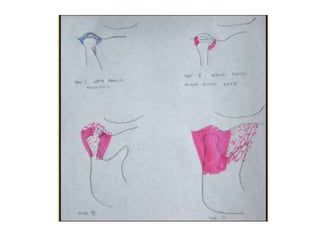
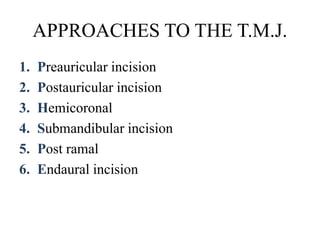
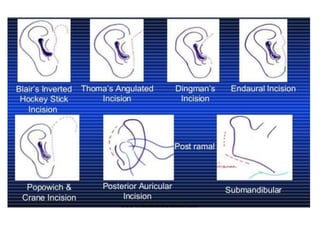
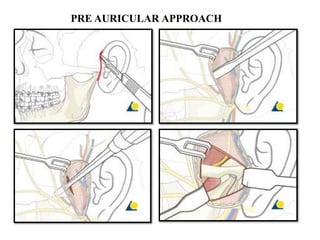
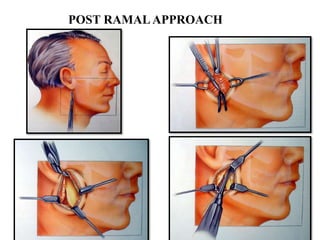
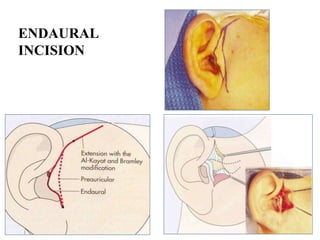
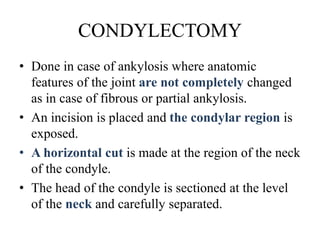
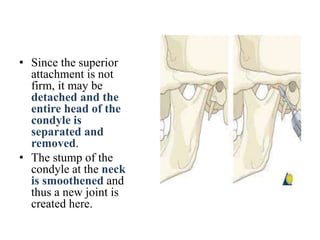
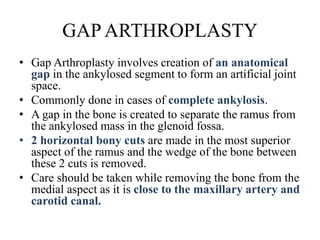
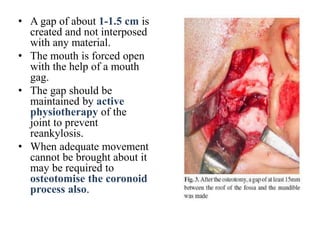
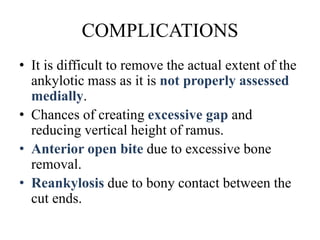
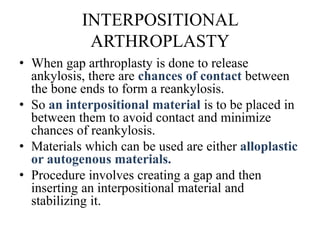
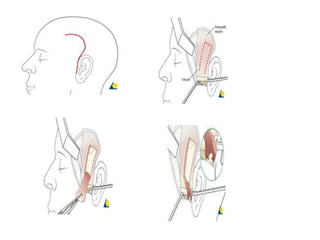
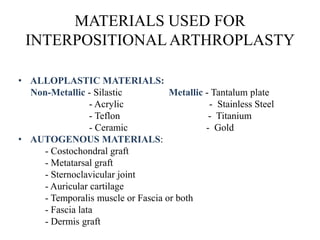
- Management involves surgical procedures like condylectomy to remove the head of the condyle, gap arthroplasty to create an artificial space, or interpositional arthroplasty using grafts to prevent re-fusion. Post-operative physiotherapy is important to maintain mobility of the joint. Complications include restricted mouth opening