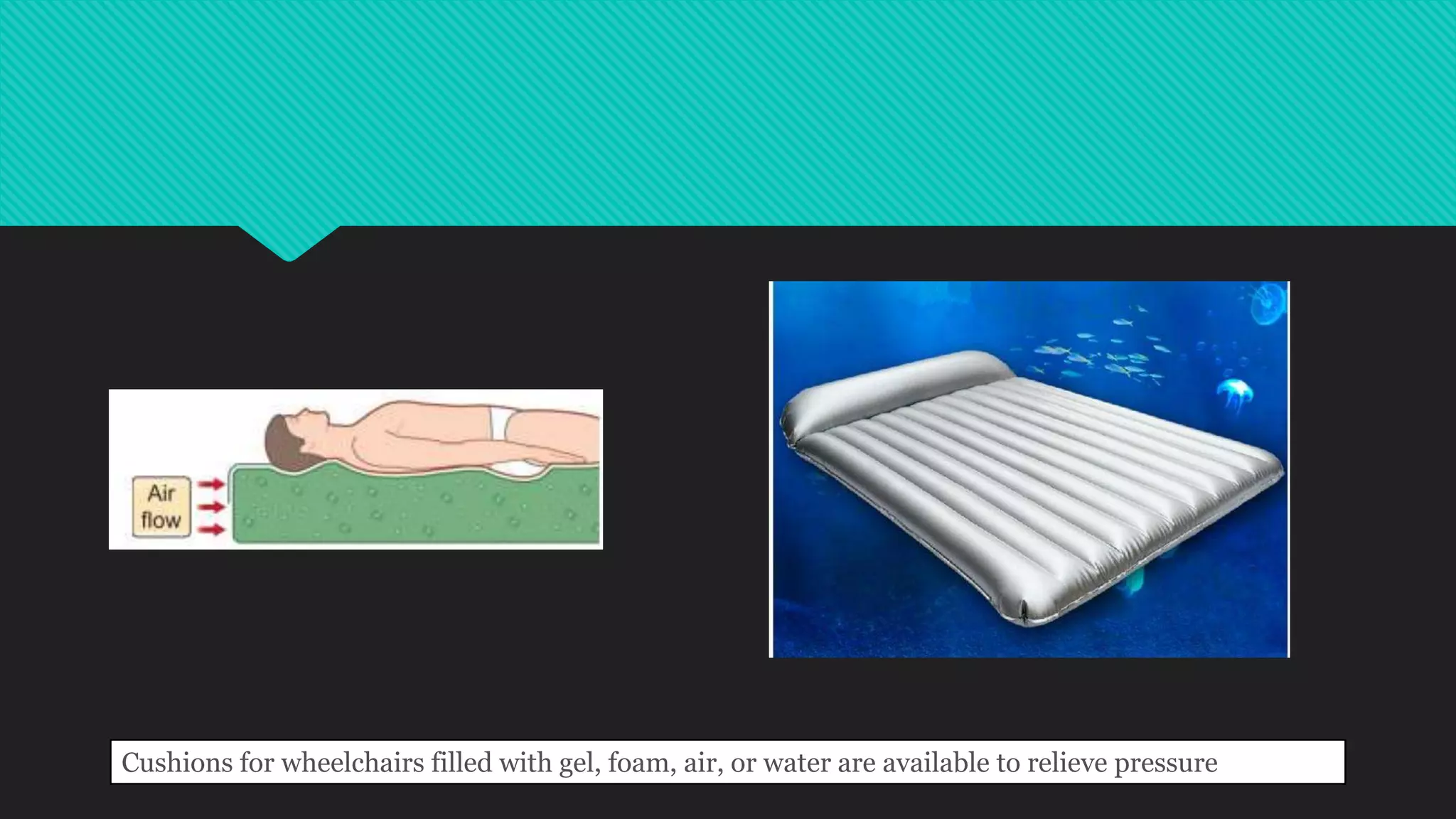
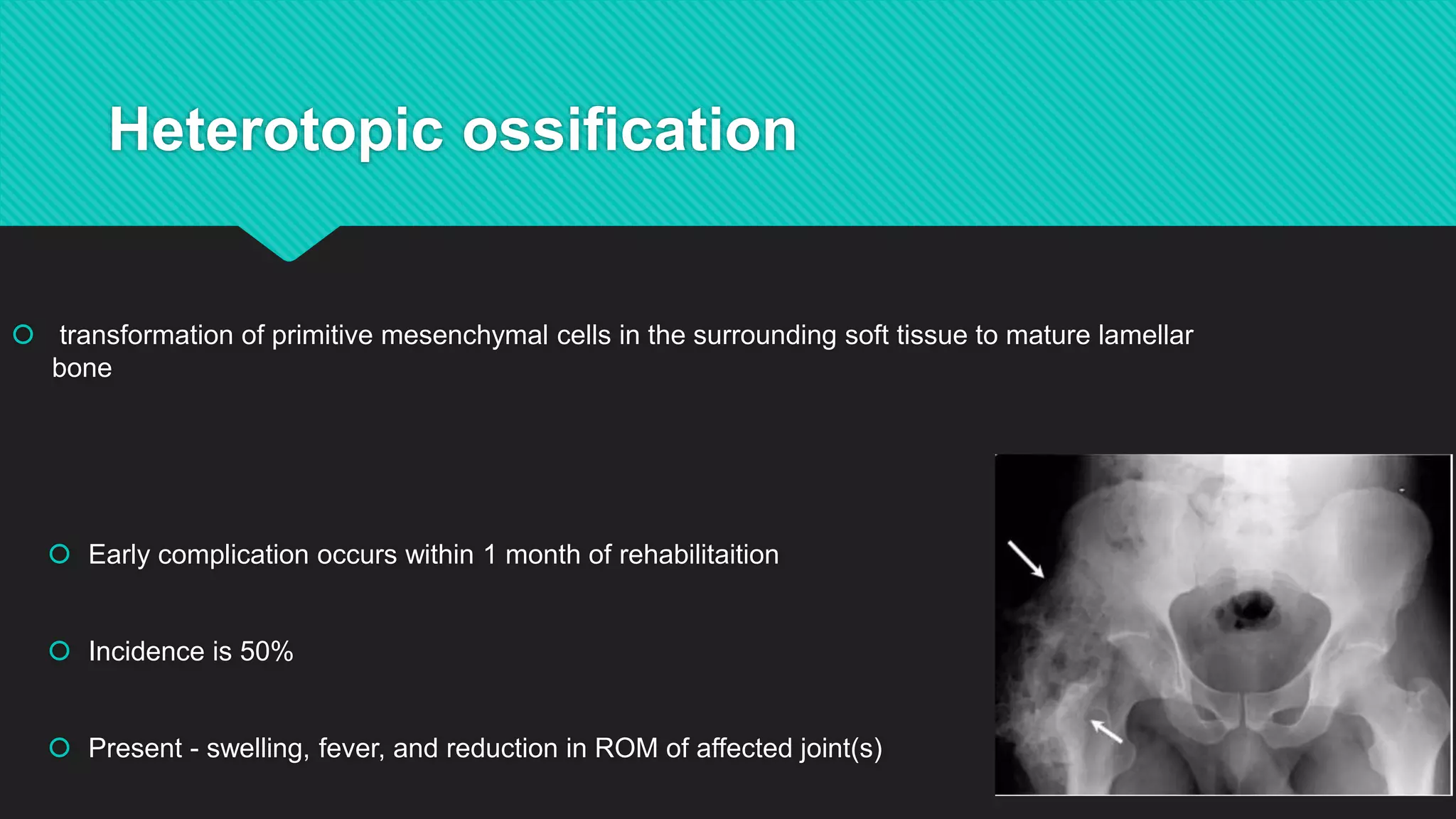
Paraplegia results from spinal cord injury and causes impairment of motor function and sensation in the lower extremities. Early rehabilitation is important to prevent secondary complications like pressure ulcers, respiratory issues, osteoporosis, urinary tract dysfunction, and others. Proper management includes preventative measures and treatments for any complications that do arise.