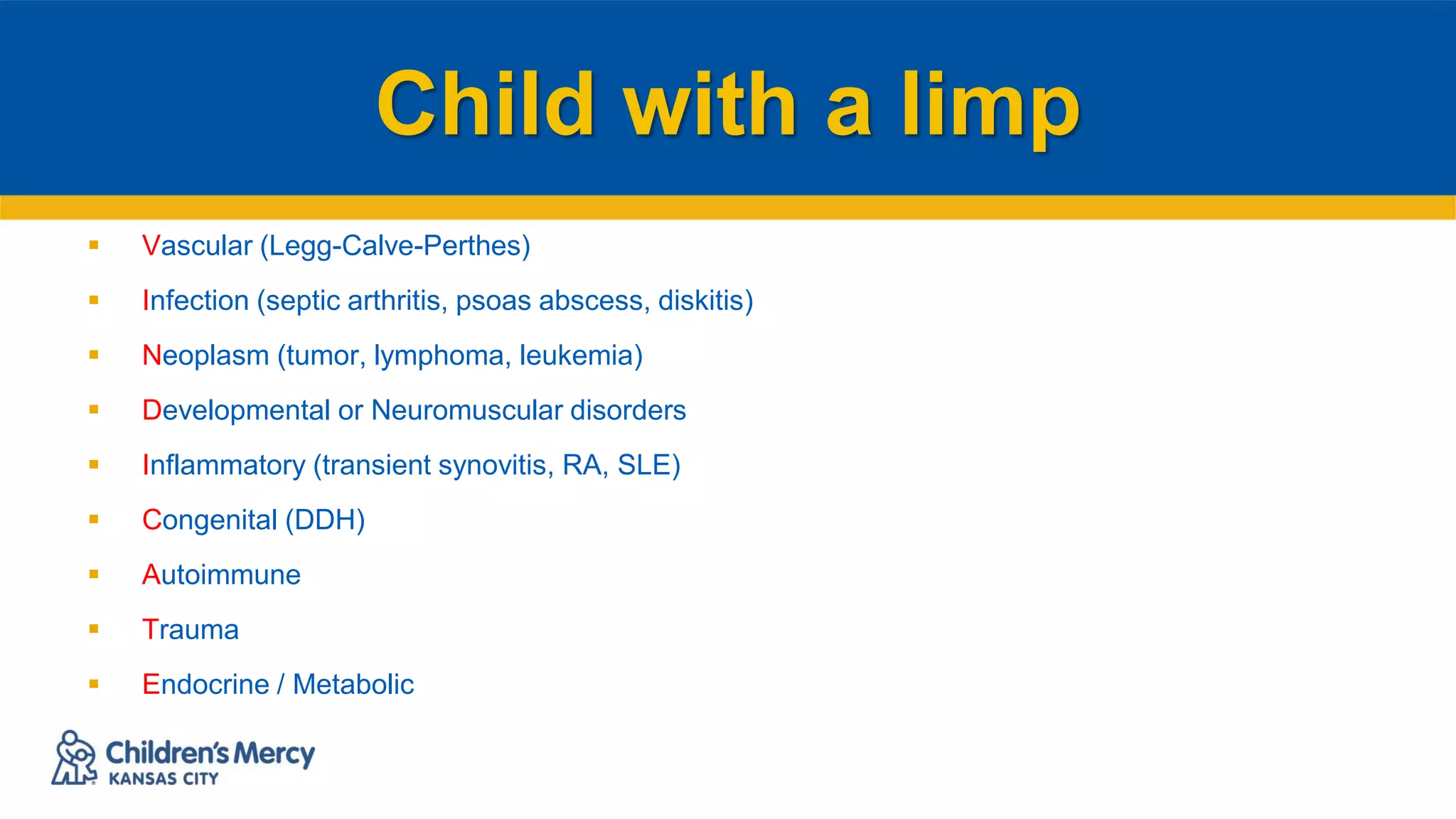
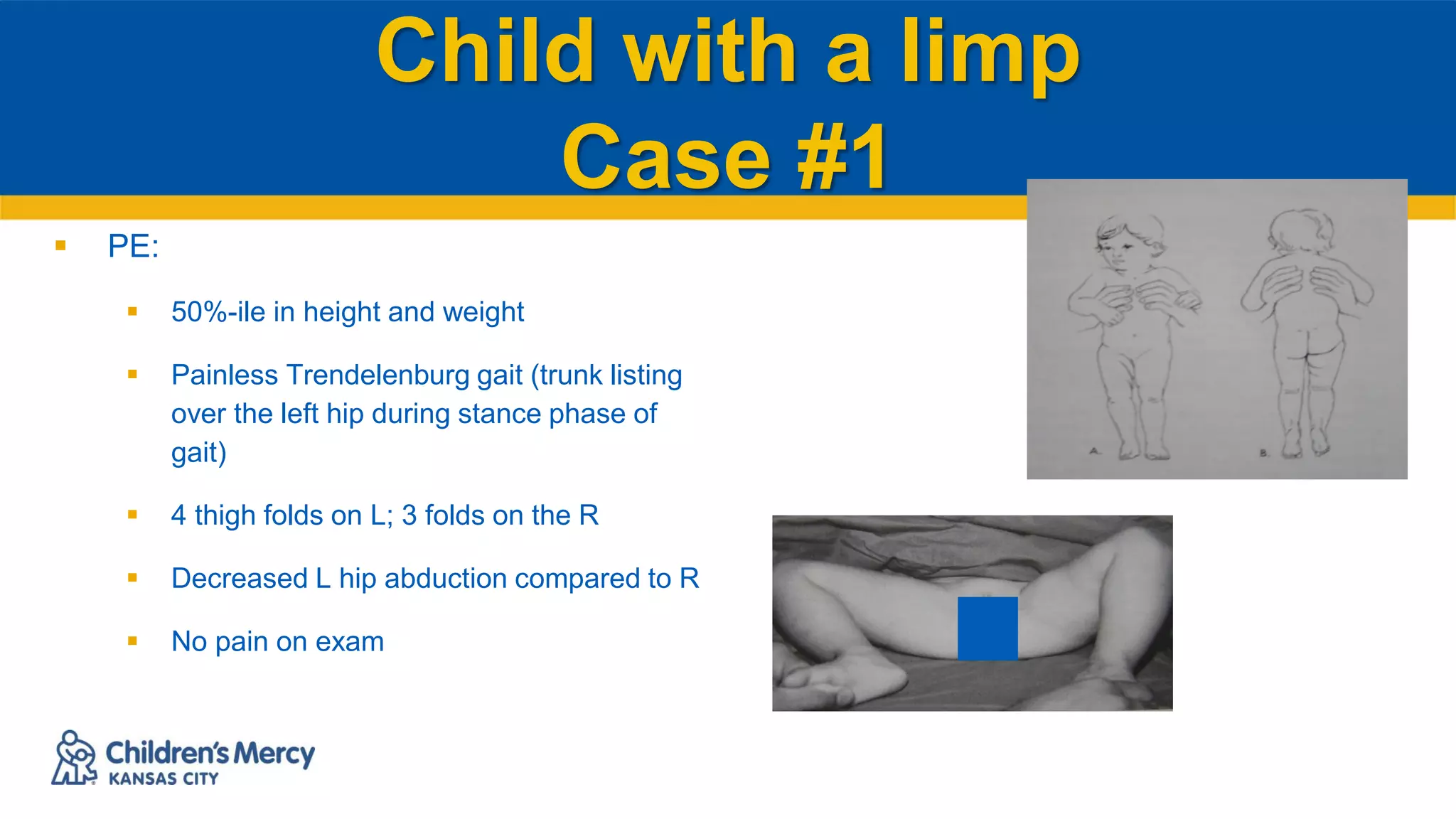
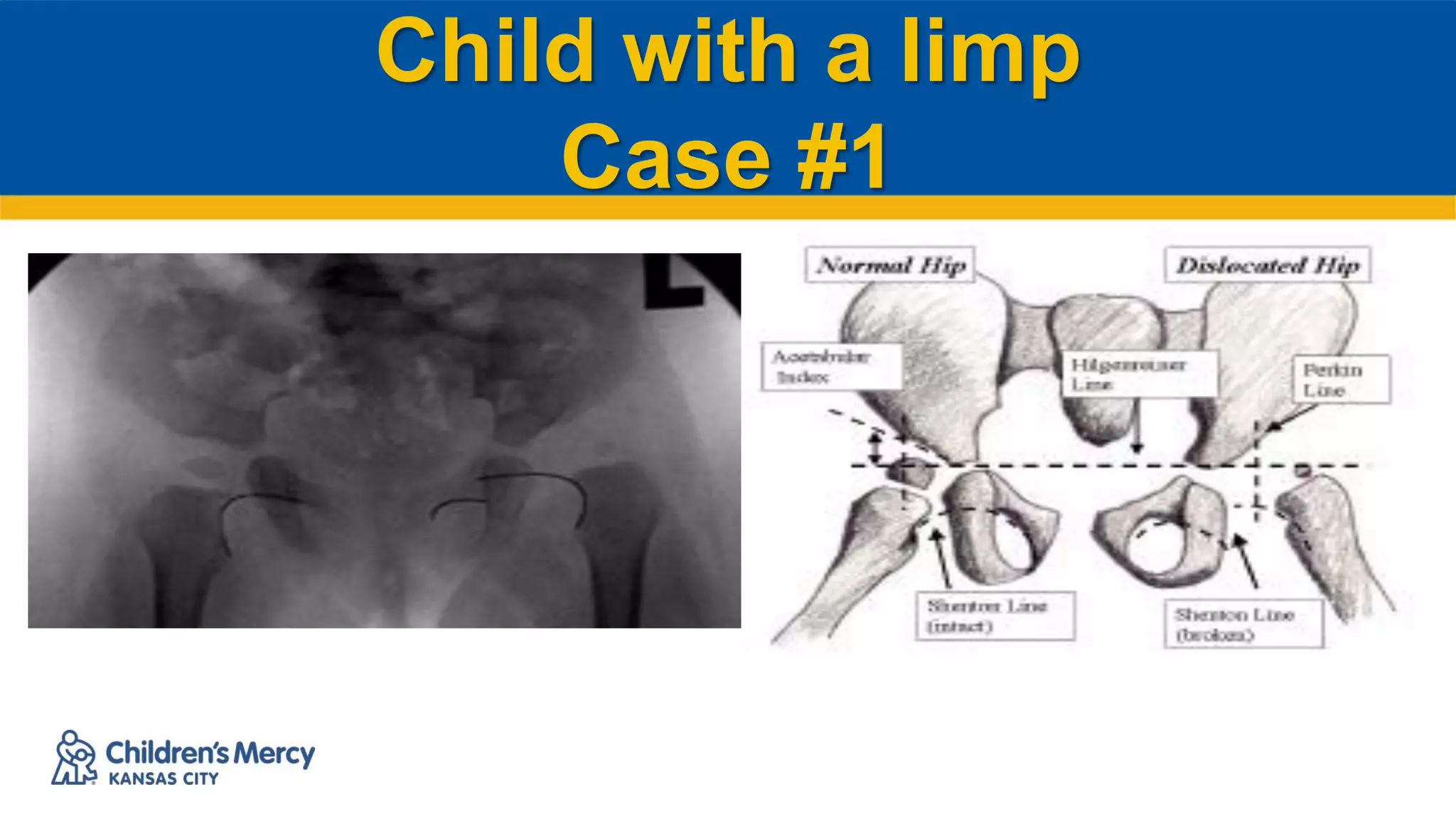
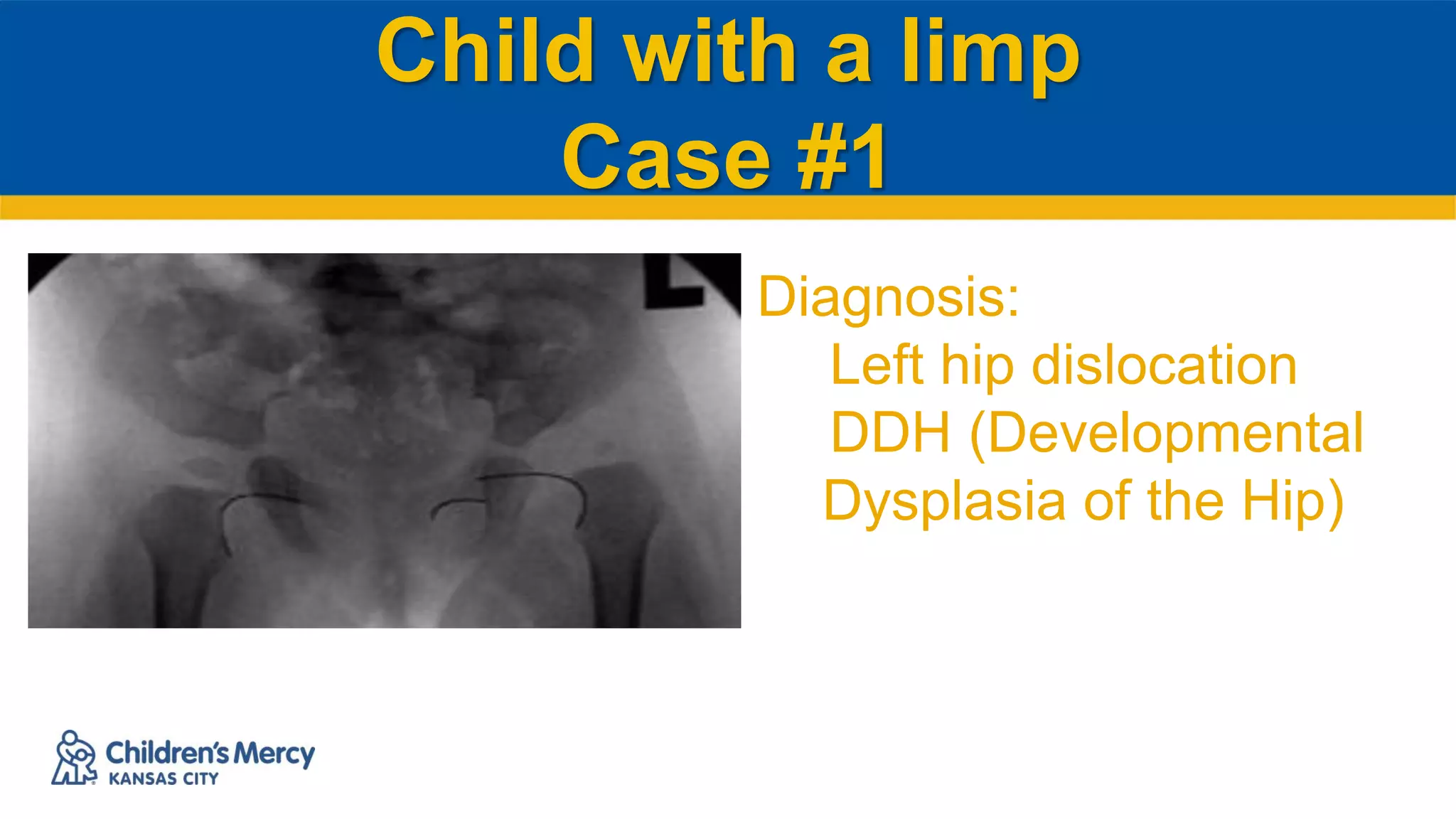
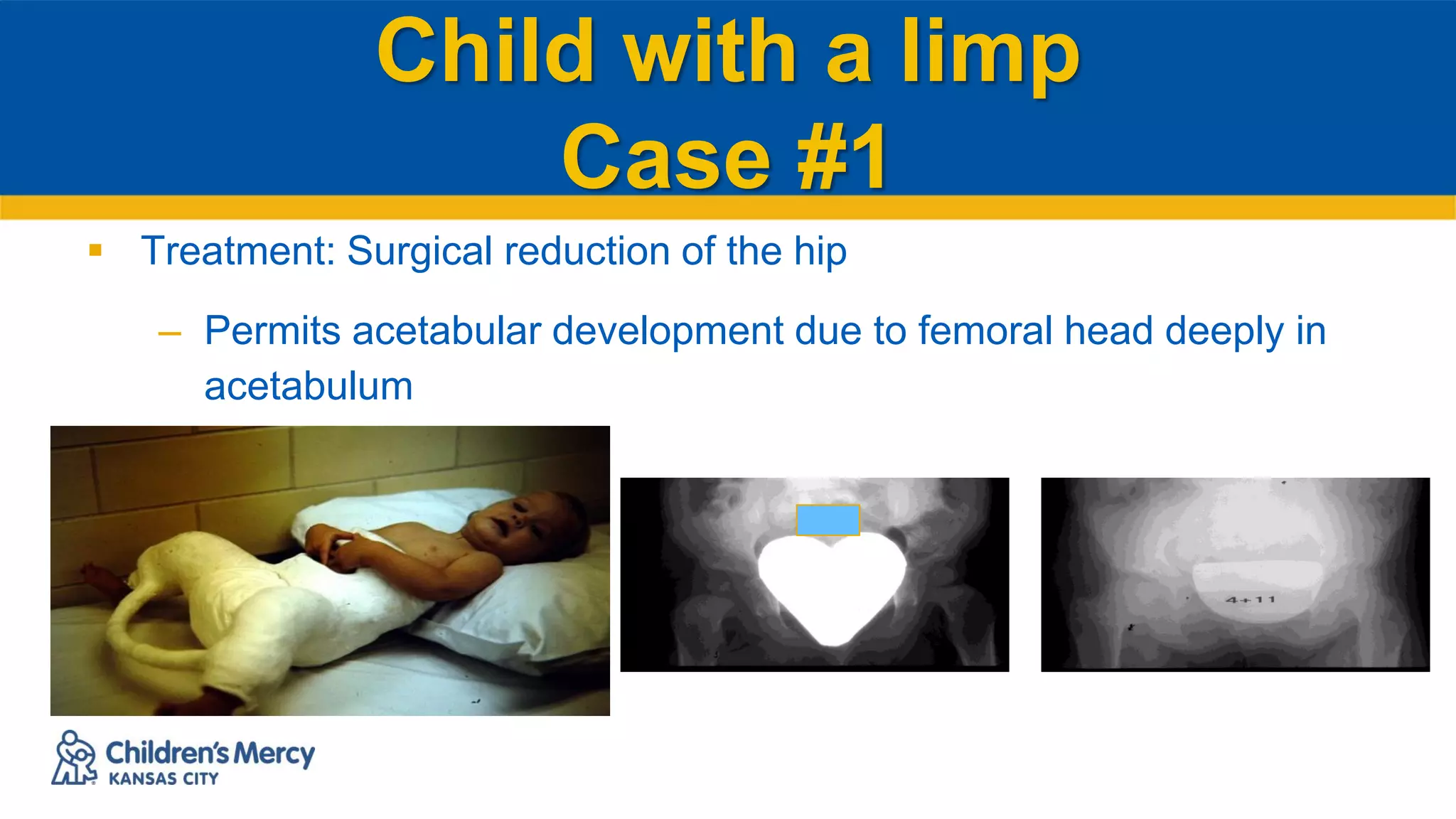
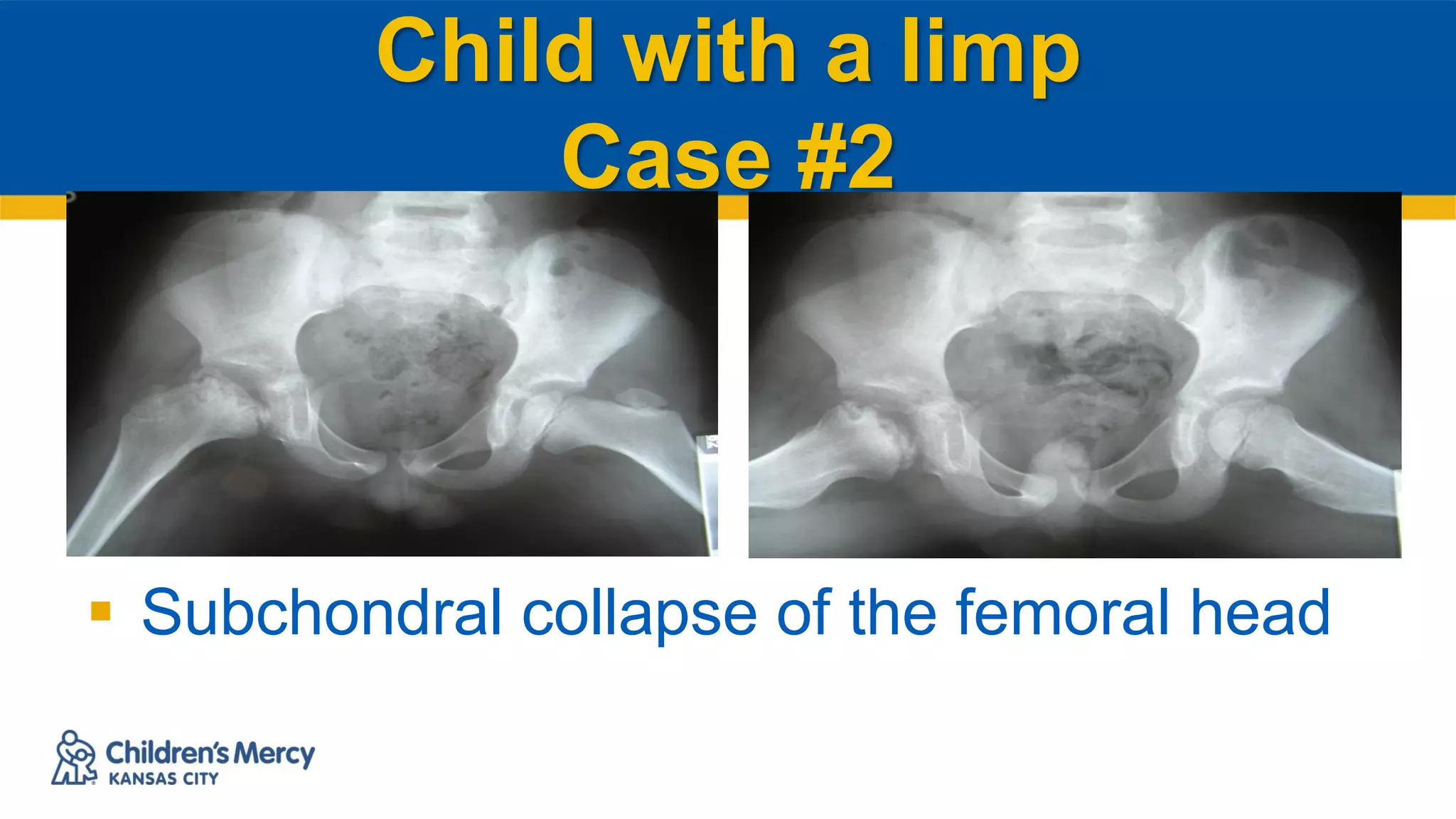
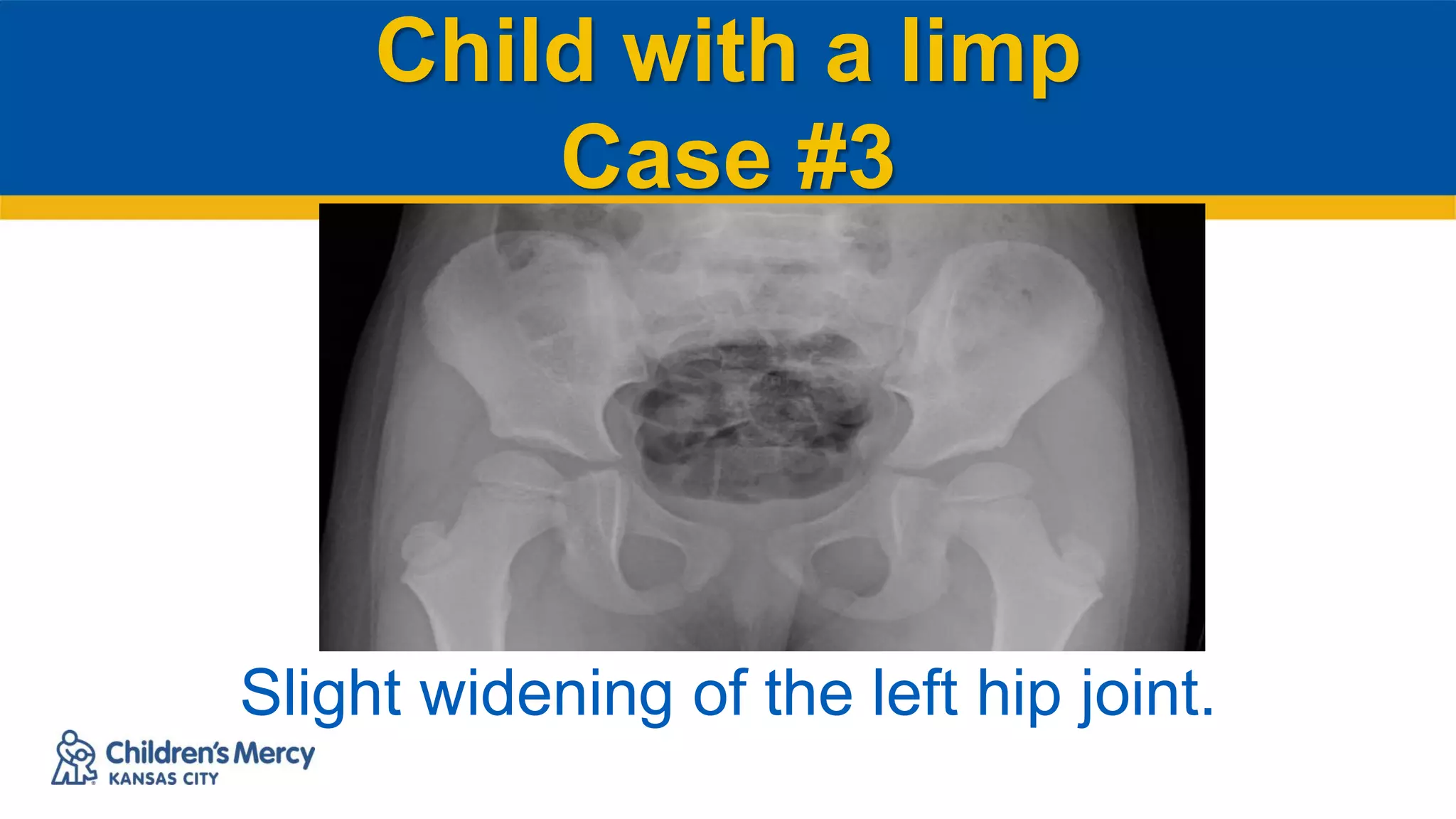
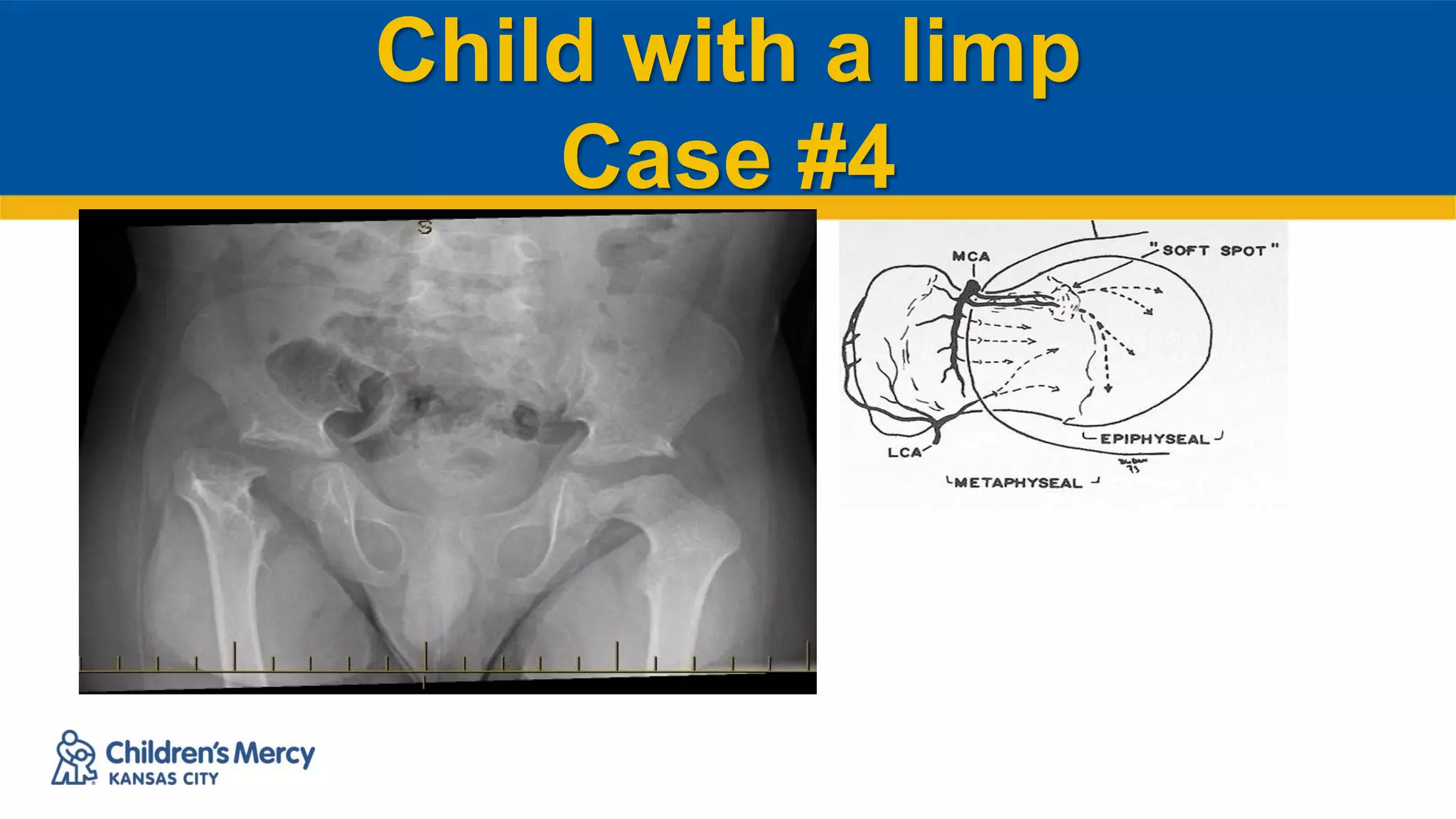
The document discusses several case examples of children presenting with a limp and the process of differential diagnosis. Case 1 involves a 18 month old with developmental dysplasia of the hip. Case 2 is a 4 year old boy diagnosed with Legg-Calve-Perthes disease. Case 3 is a 4 year old girl with transient synovitis of the hip.