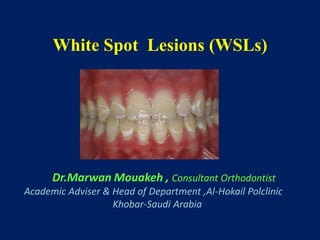
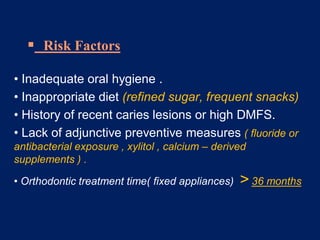
White spot lesions (WSLs) are decalcifications of enamel adjacent to orthodontic appliances, prevalent during orthodontic treatment and associated with plaque accumulation and factors such as poor oral hygiene and diet. The document outlines the classification, prevalence, etiology, and prevention strategies for WSLs, emphasizing the importance of maintaining oral hygiene and using fluoride. It also discusses treatment options ranging from natural remineralization to more aggressive interventions like microabrasion or cosmetic restorations for established lesions.