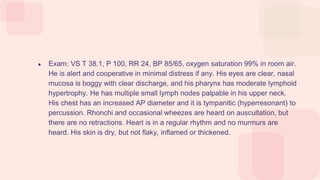
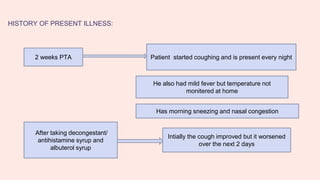
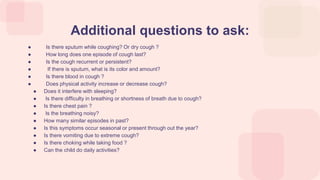
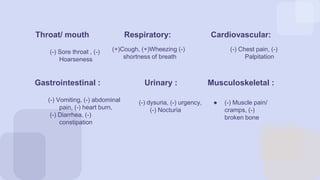
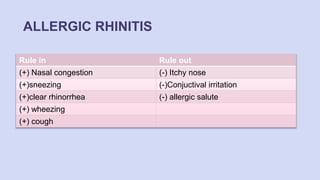
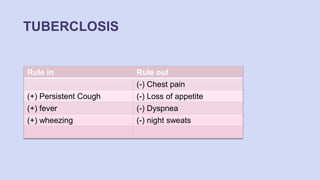
A 3-year-old boy presents with a 2-week history of nightly coughing, mild fever, morning sneezing, and nasal congestion, alongside a past history of eczema and a family history of asthma. Physical examination reveals boggy nasal mucosa, moderate lymphoid hypertrophy, and wheezing, leading to a diagnosis of moderate persistent childhood asthma. Management includes education on asthma control, daily inhaled corticosteroids, and steps to avoid triggers and allergens.