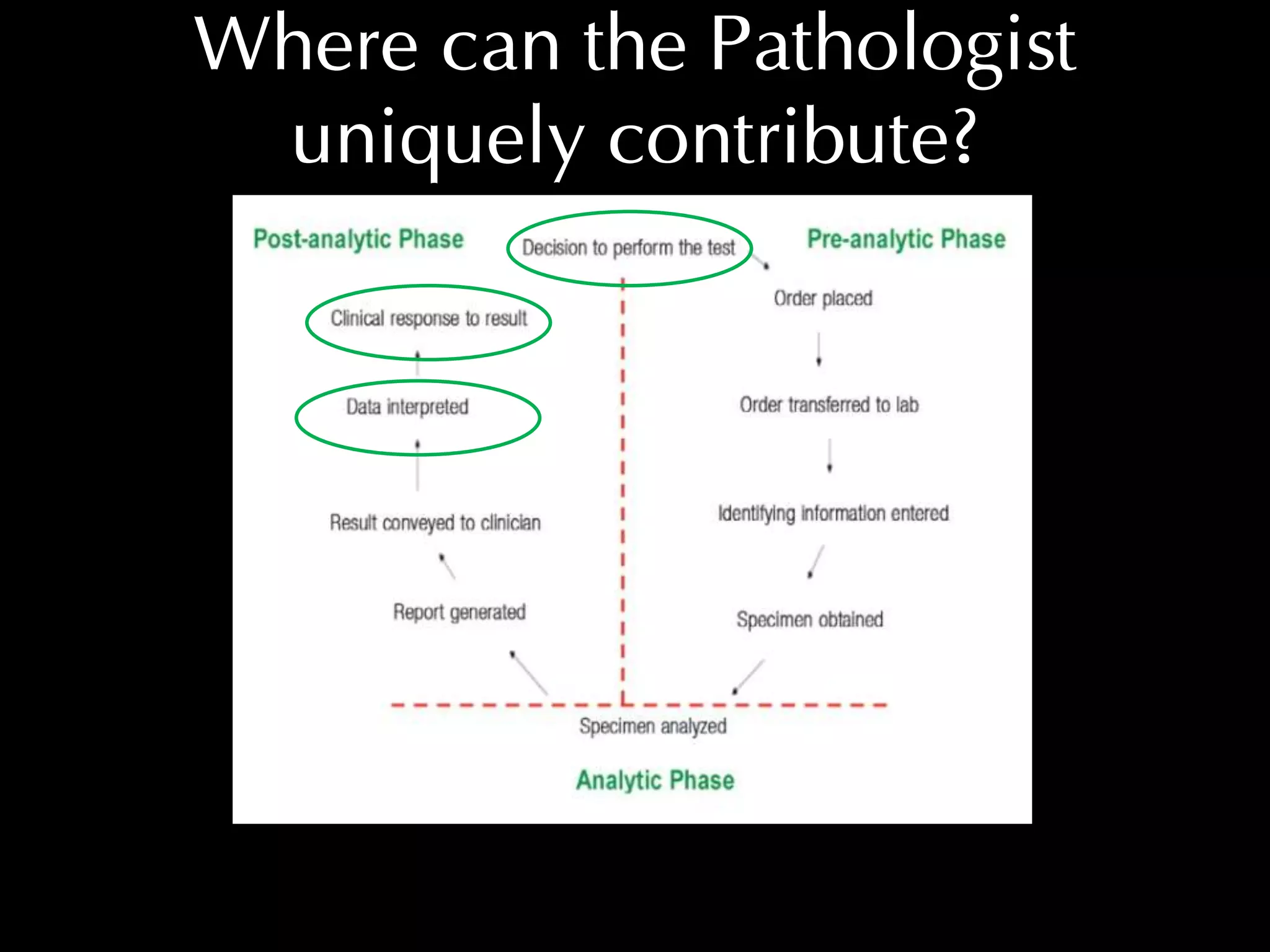
The role of the pathologist in clinical pathology is to oversee the laboratory testing cycle and provide guidance to clinicians. Pathologists can uniquely contribute by:
1) Guiding clinicians on appropriate test selection from the large test menu.
2) Guiding appropriate testing to avoid unnecessary tests that increase the risk of false positives.
3) Interpreting laboratory results in the proper clinical context since primary data can be uninformative without considering the clinical scenario.