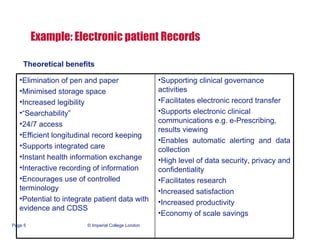
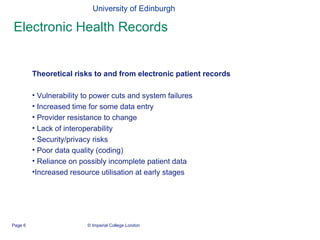
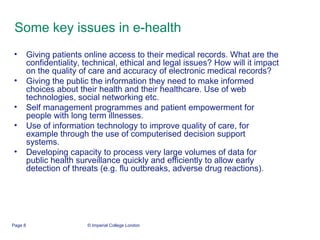
The document discusses e-health and some of the key issues surrounding it. It notes that e-health has the potential to increase efficiency and quality of care by reducing costs and variations while supporting things like remote access and data sharing. However, implementation also carries risks like technical failures, integration issues, and privacy/security concerns. Overall, while the theoretical benefits are clear, more evidence is still needed to demonstrate the actual impacts and address human/cultural factors.