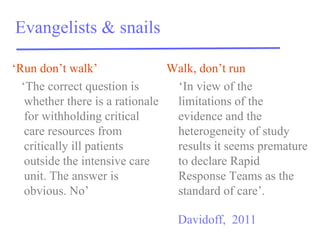
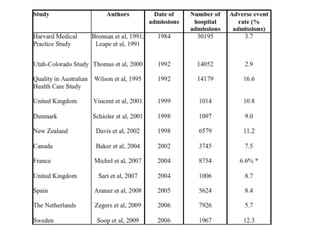
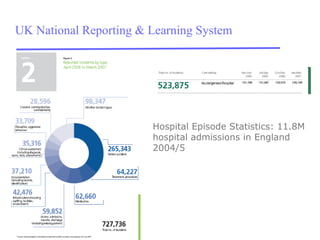
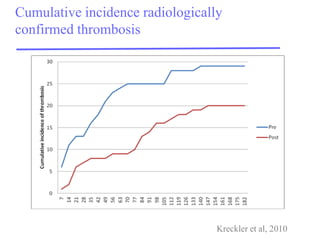
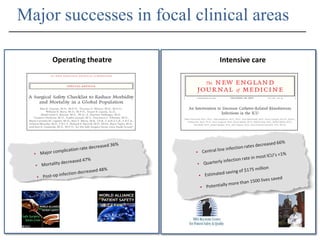
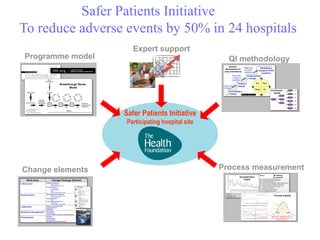
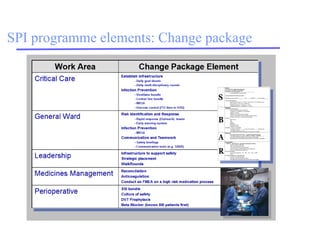
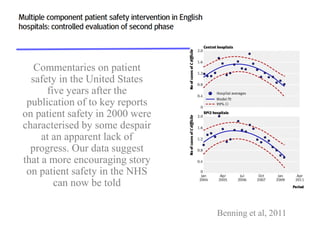
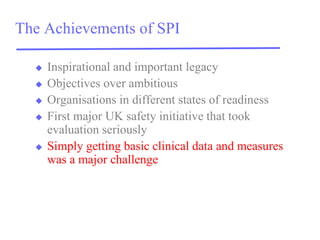
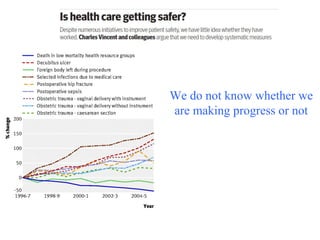
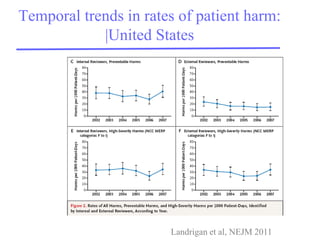
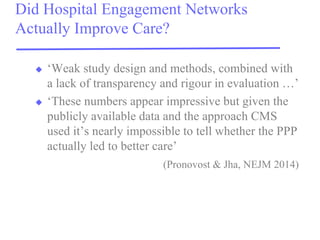
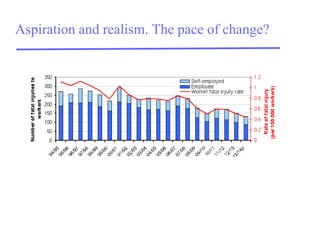
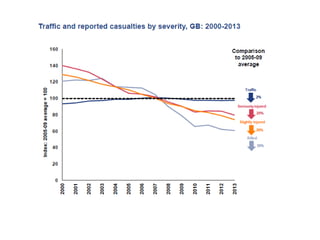
The document discusses the progress and challenges in improving patient safety in healthcare, particularly within the NHS, highlighting initiatives like the Safer Patients Initiative that aim to reduce adverse events by 50%. Despite some success in reducing hospital-acquired conditions, the document points out issues with engagement networks and measurement of progress, stressing the importance of rigorous evaluation. Overall, while some encouraging trends are noted, there's still a significant need for improvement and accountability in patient safety measures.