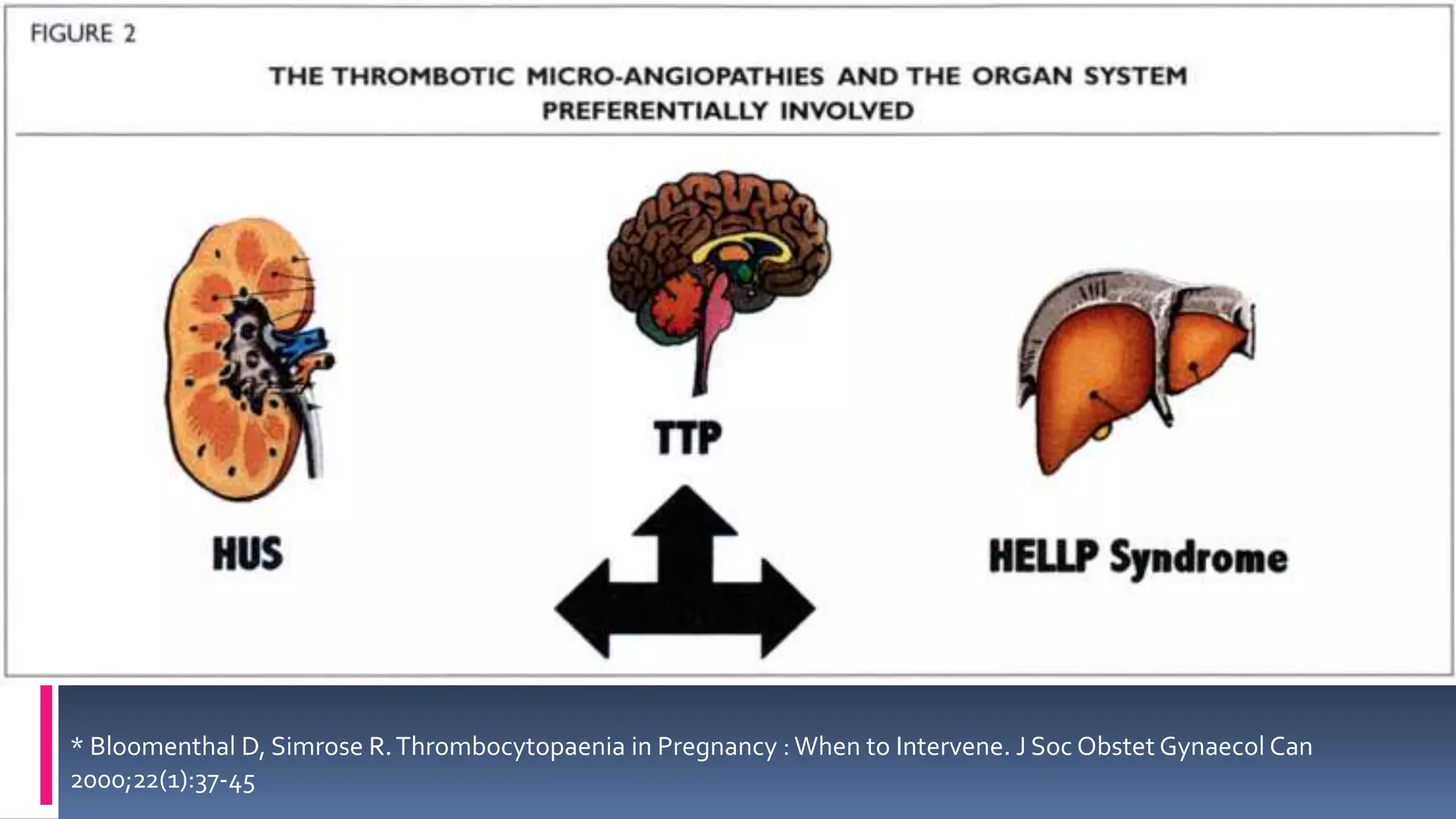
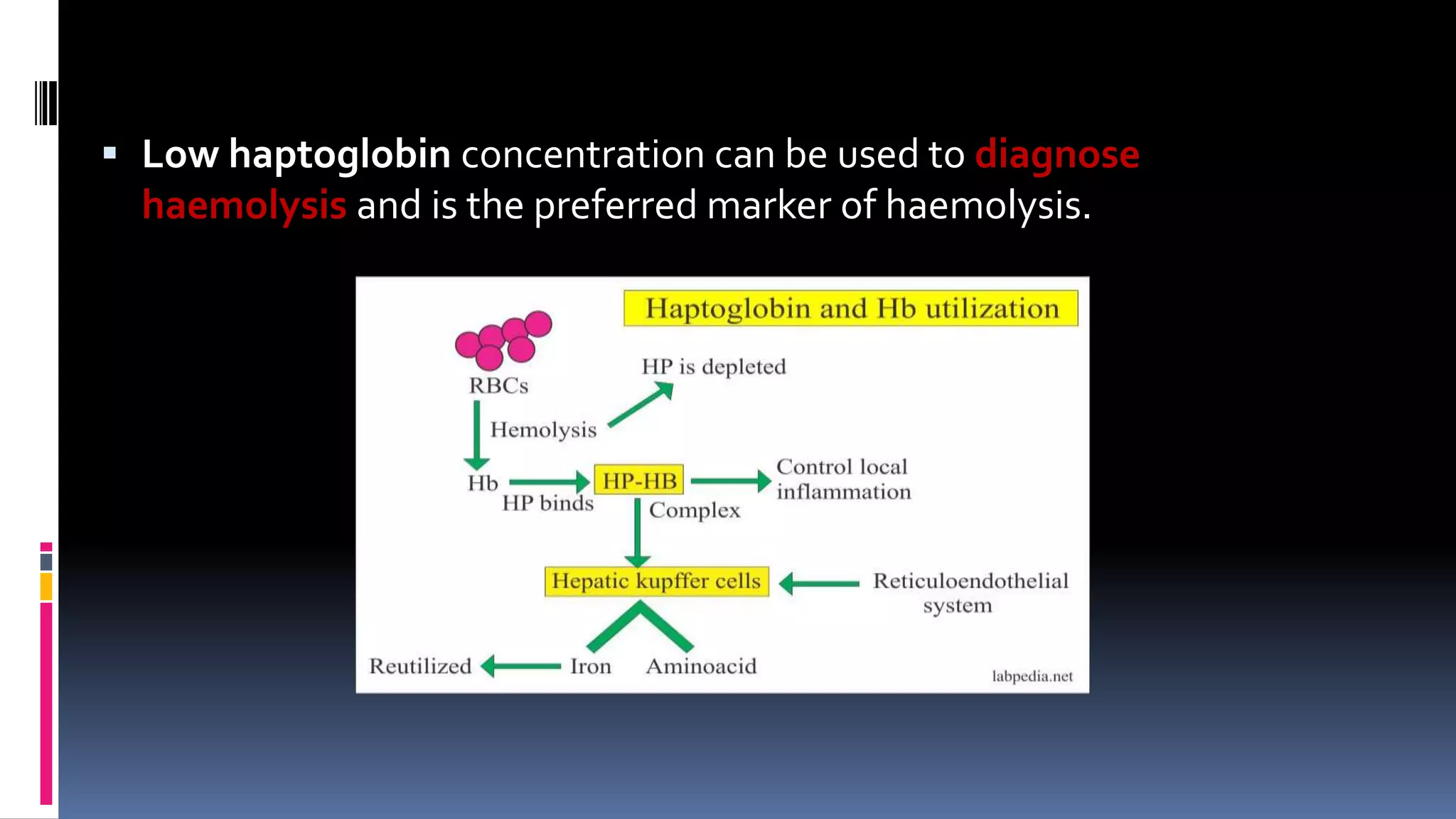
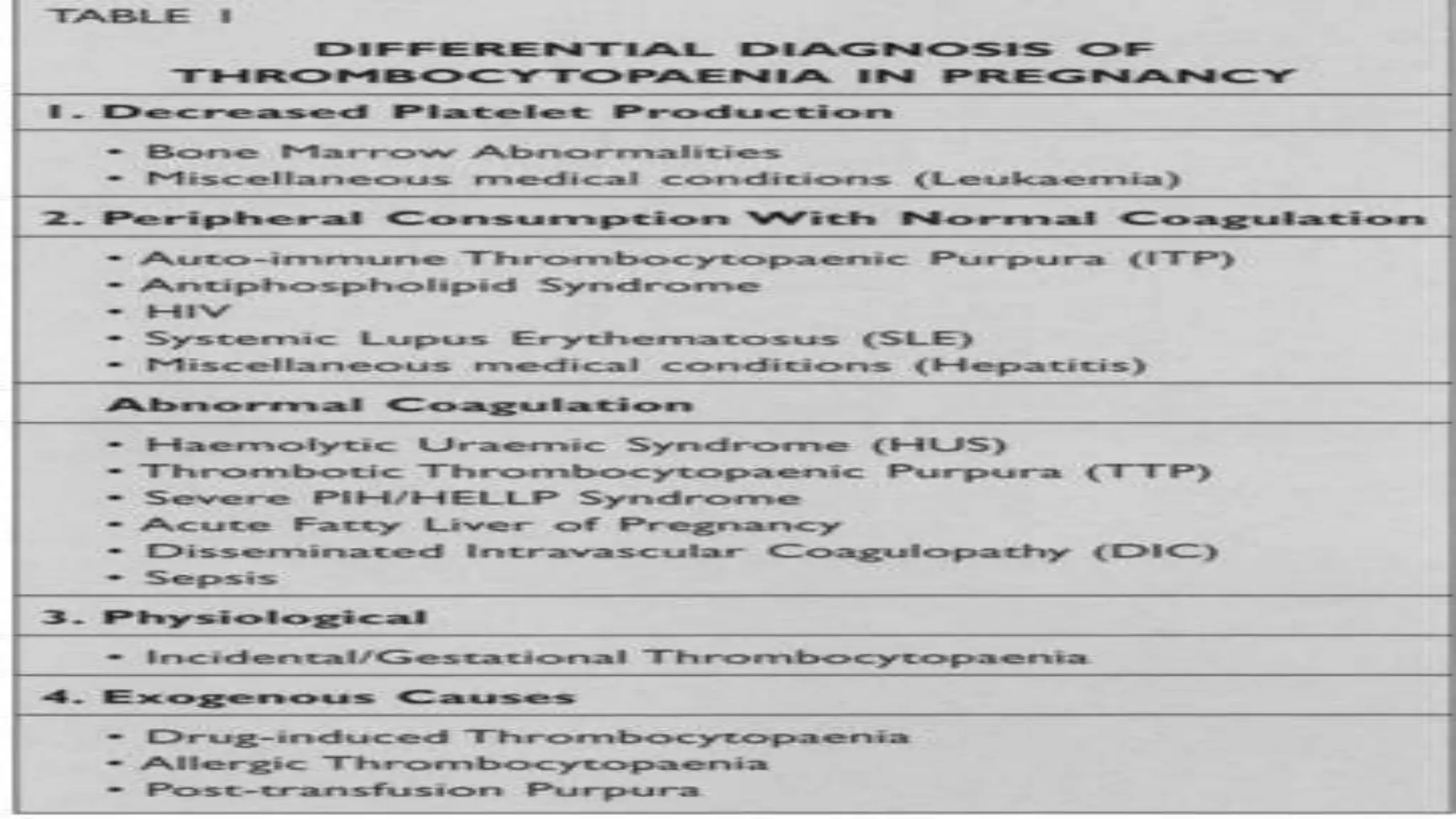
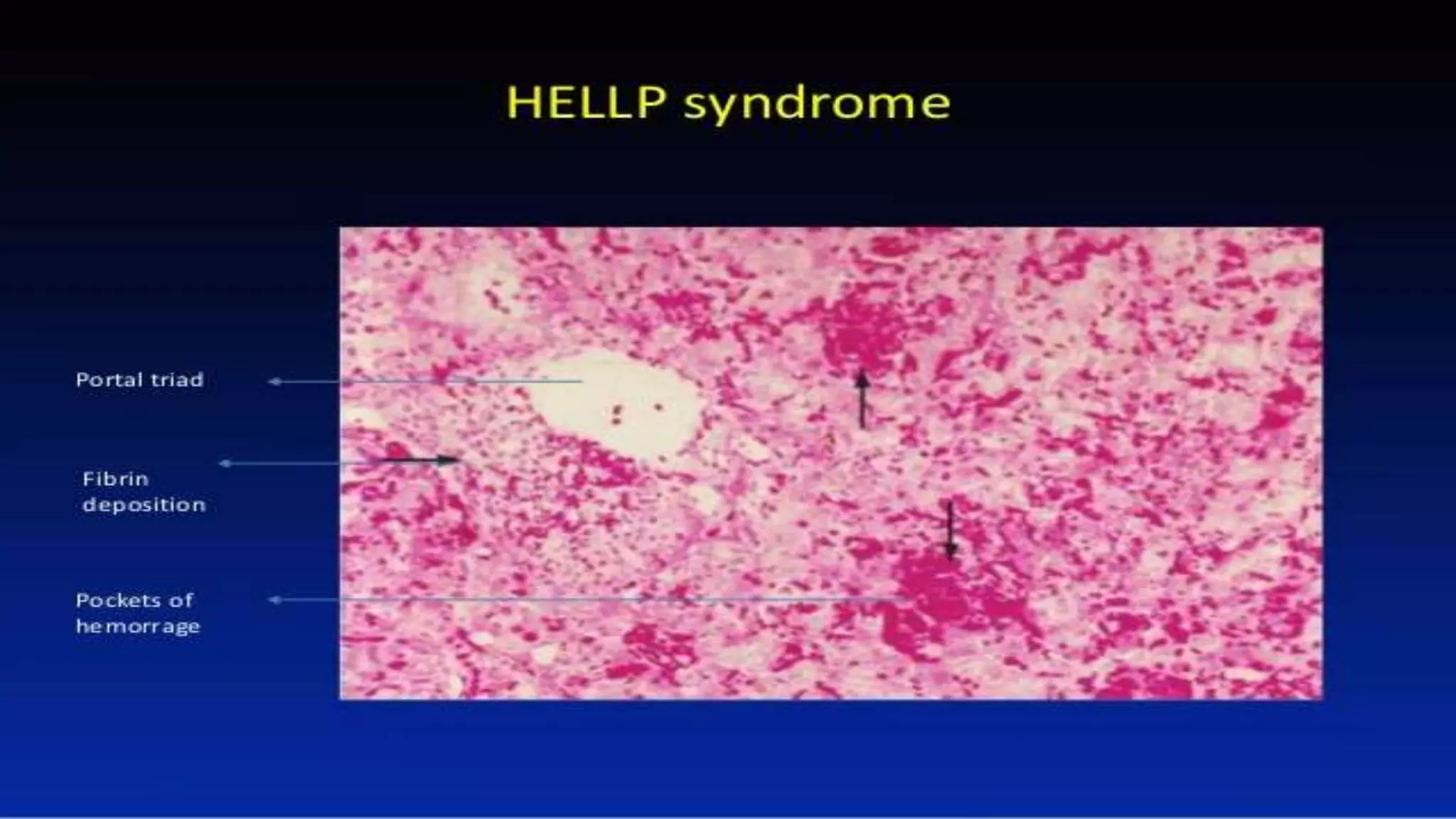
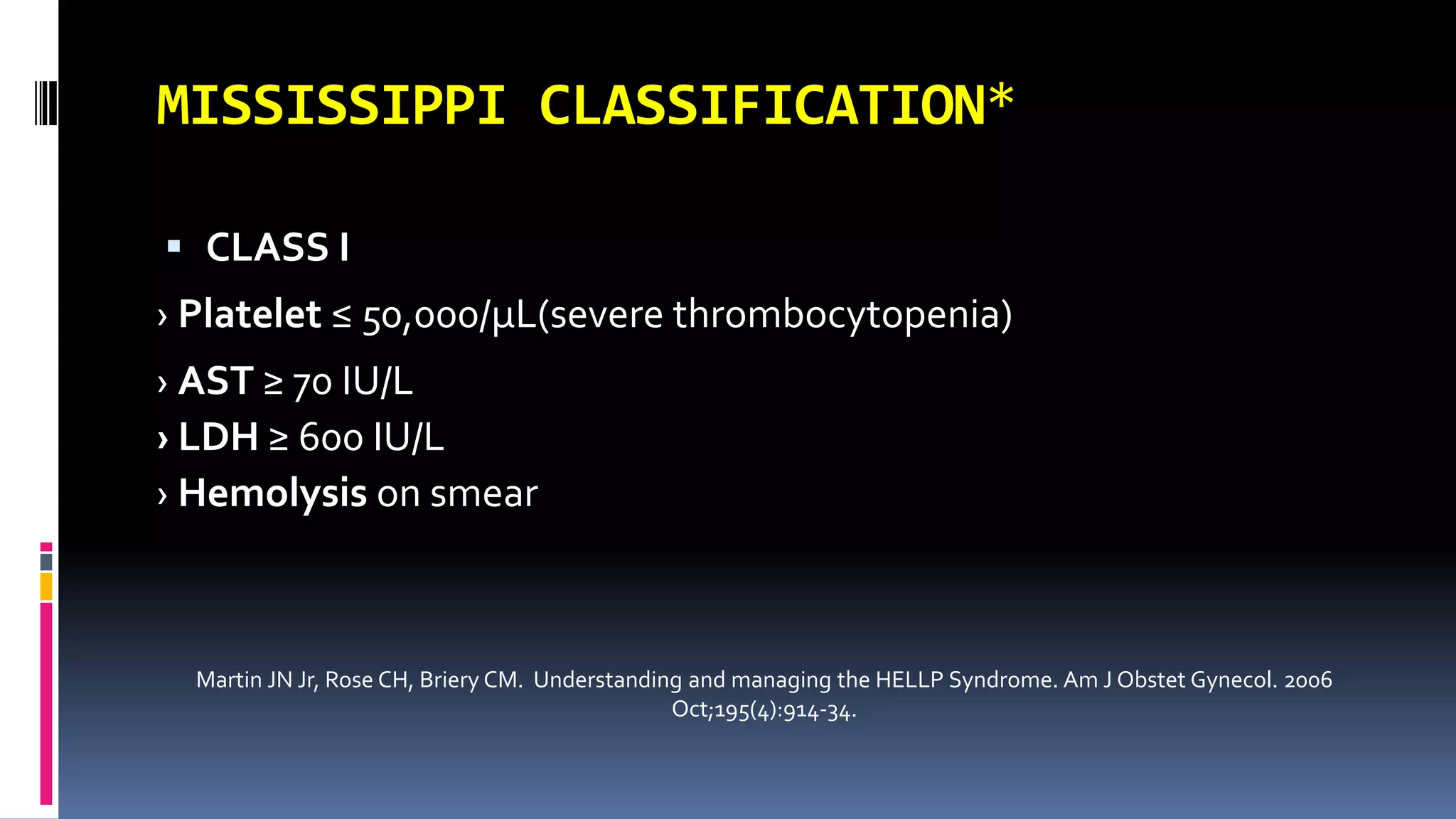
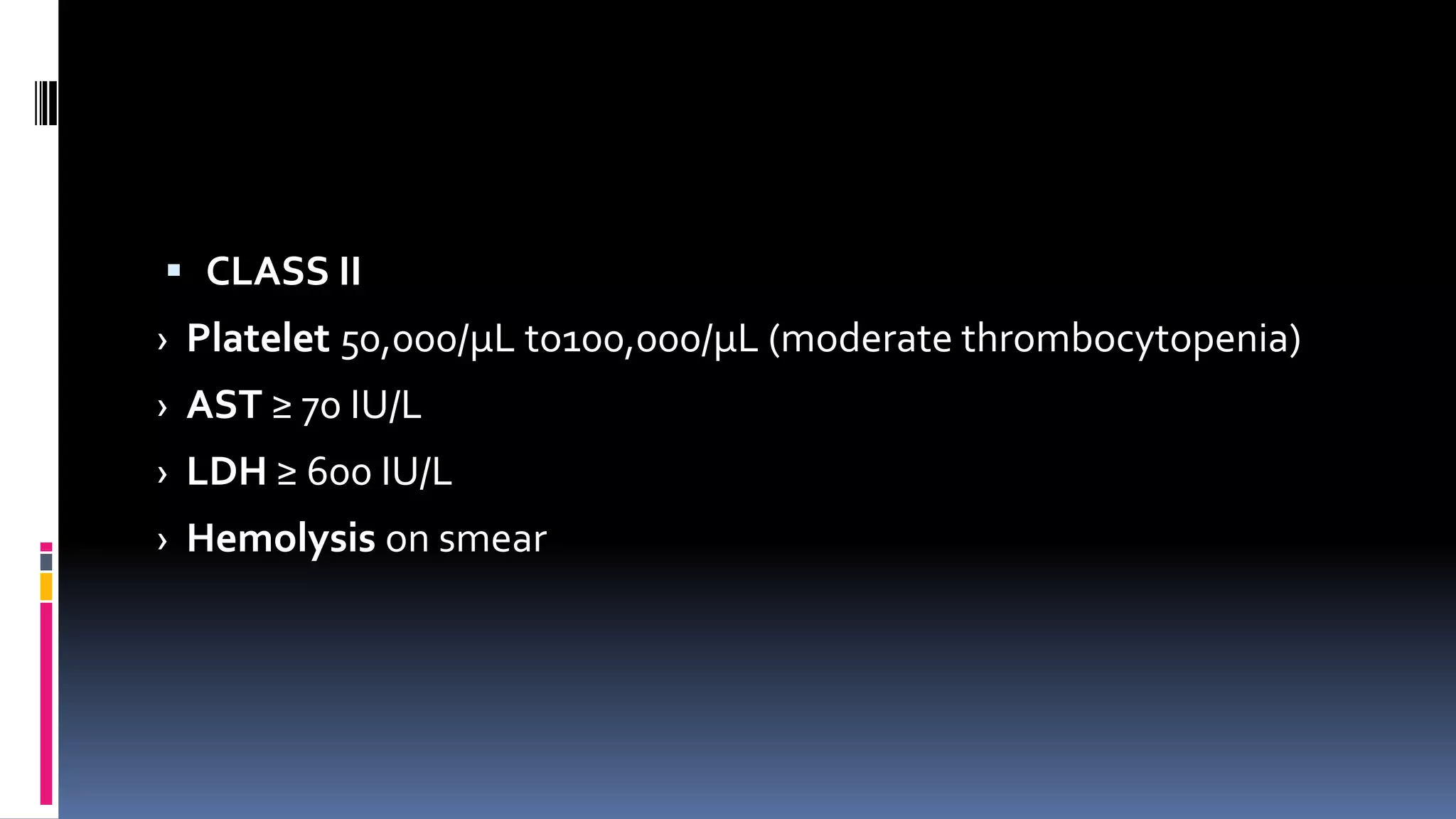
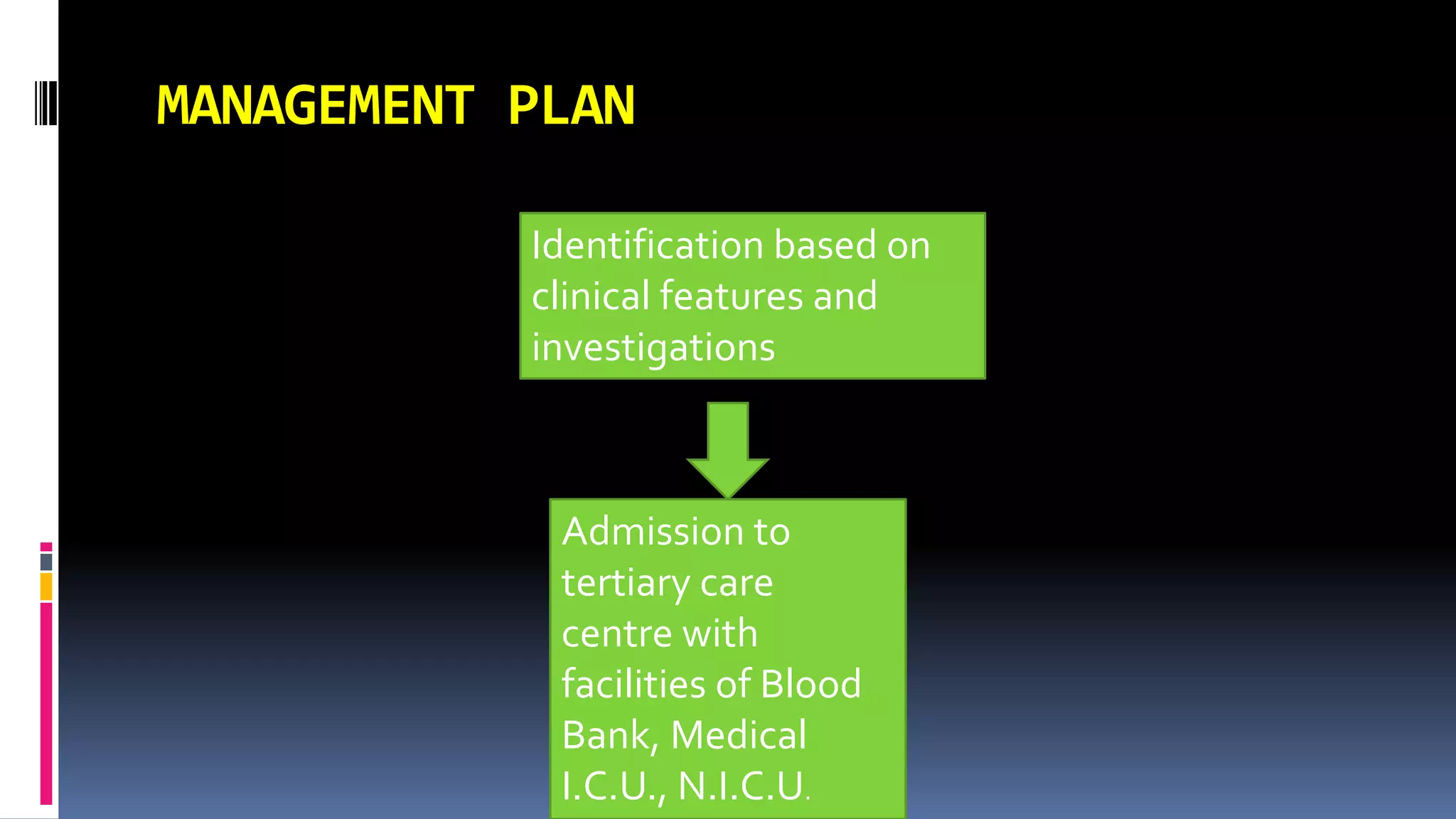
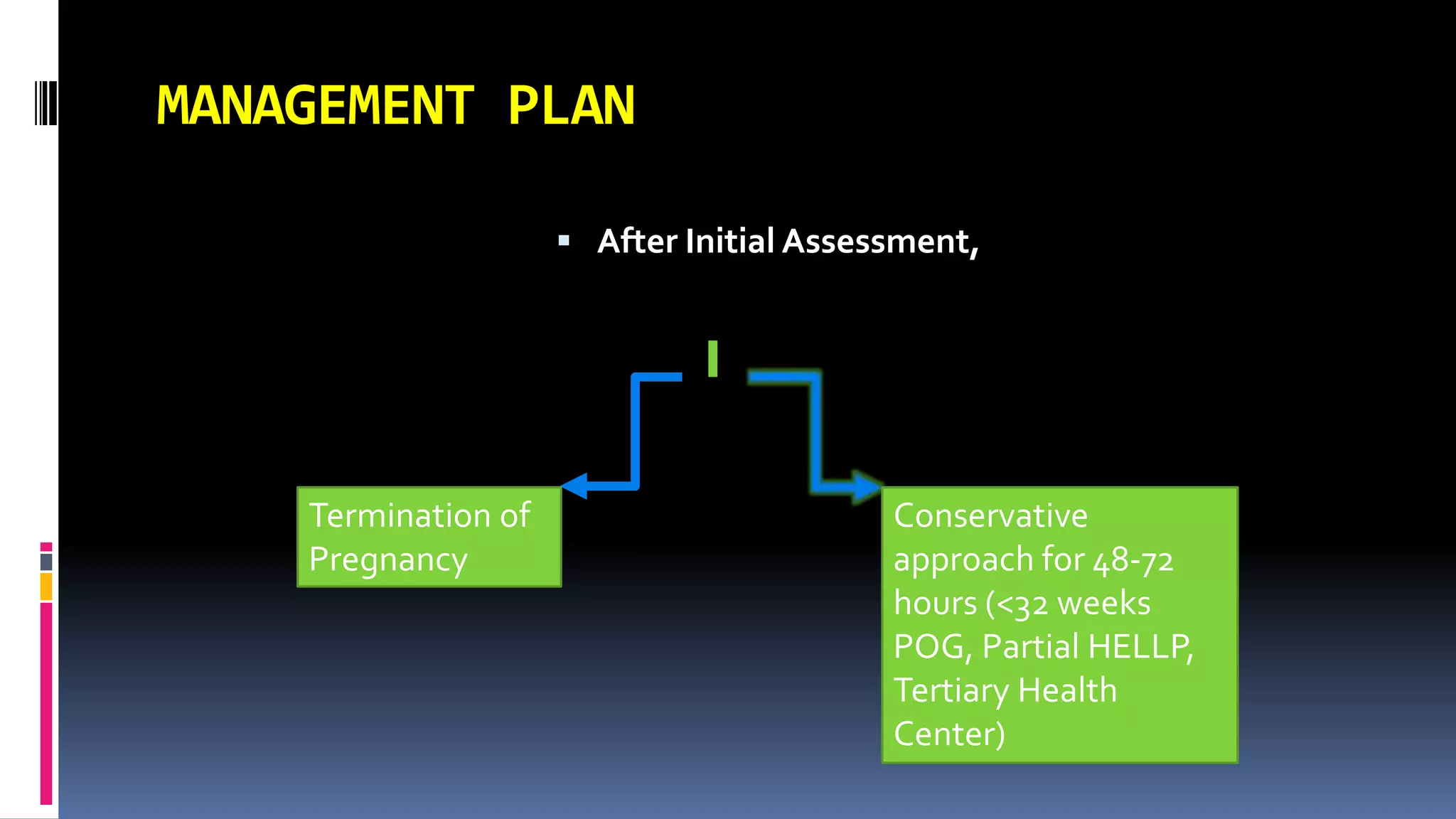
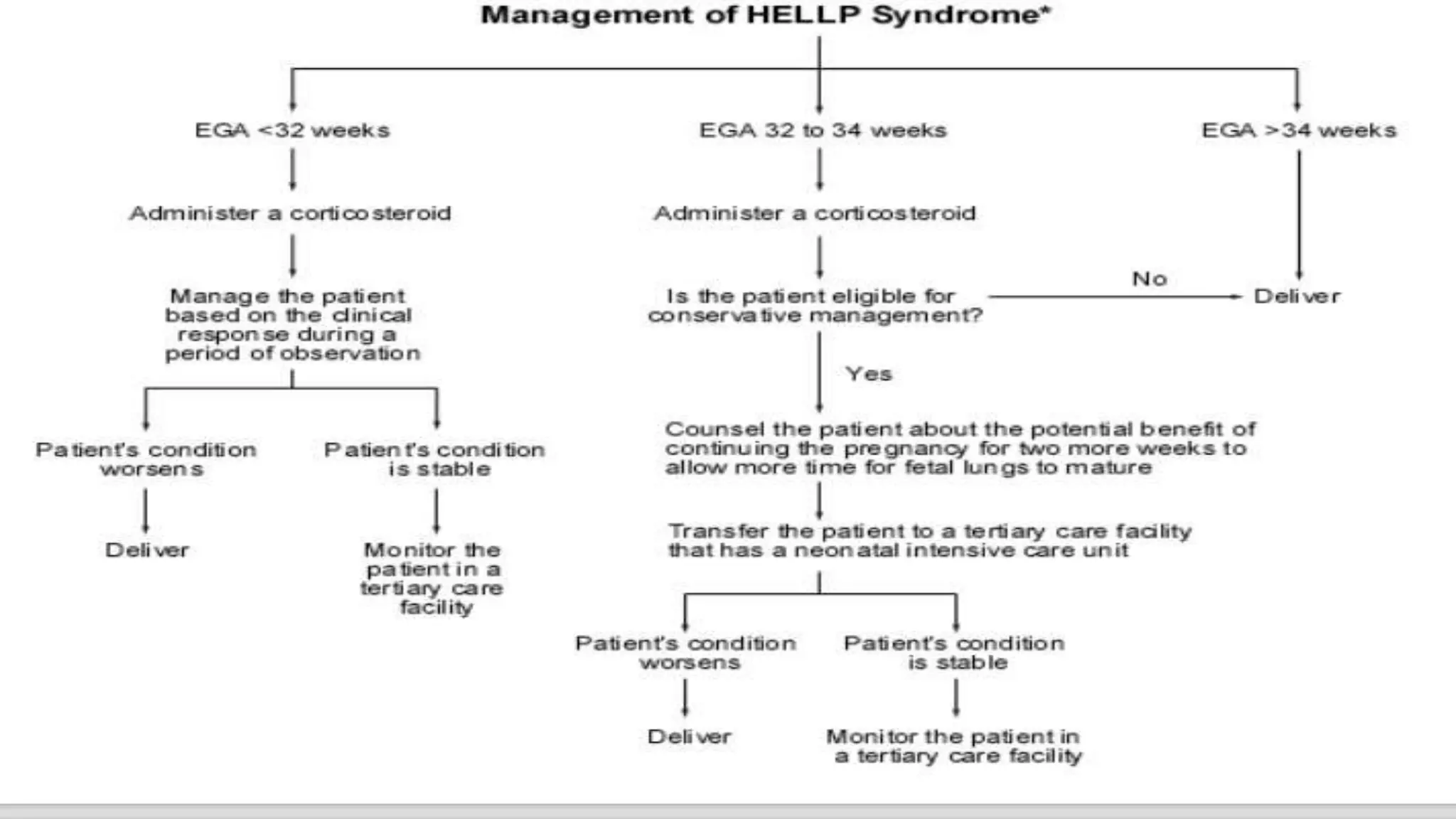
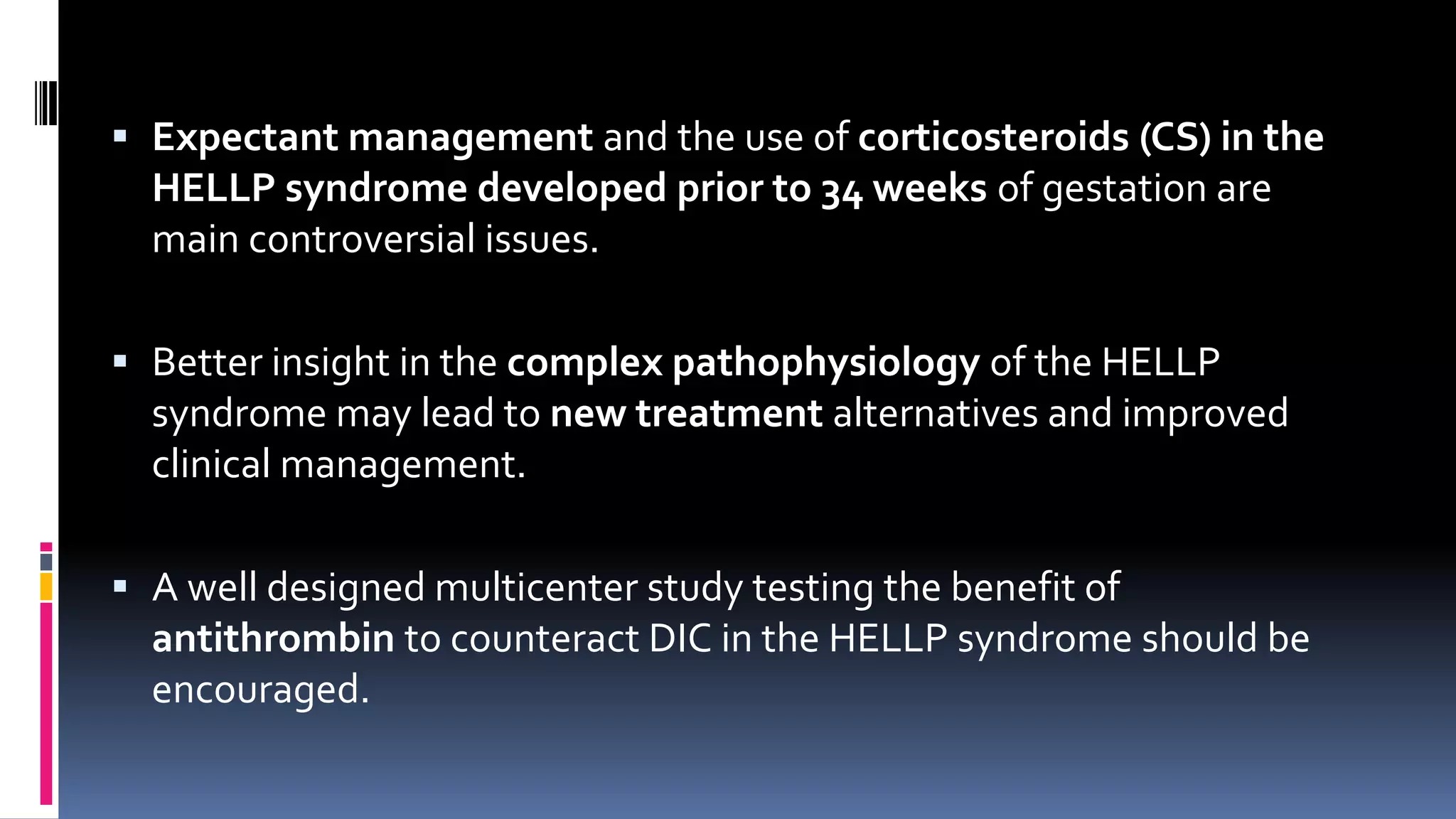
HELLP syndrome is a life-threatening variant of preeclampsia characterized by hemolysis, elevated liver enzymes, and low platelet count. It is caused by endothelial dysfunction and damage. Management involves careful monitoring, stabilization, and prompt delivery between 24-34 weeks with corticosteroid administration to improve fetal outcomes. Delivery is indicated after 34 weeks, while expectant management may be considered before 27 weeks with close monitoring.