This document discusses vocal cord paralysis, including its causes, symptoms, diagnosis, and treatment options. Some key points:
- Vocal cord paralysis can impair breathing, swallowing, and voicing. Common symptoms are breathy voice and difficulty swallowing liquids.
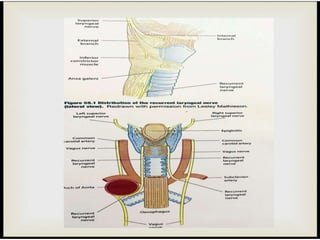
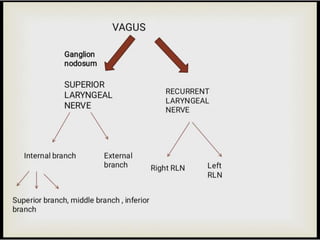
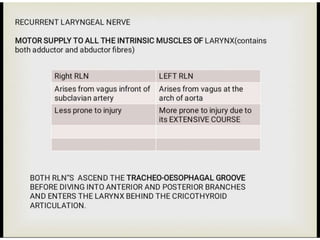
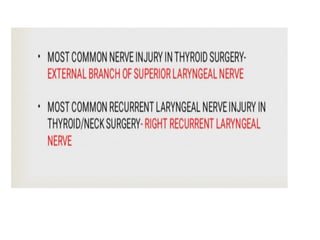
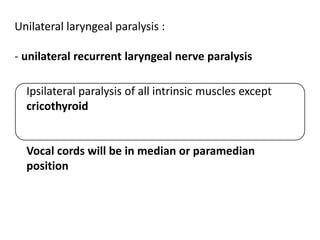
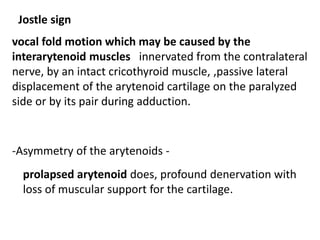
- It is usually caused by damage to the recurrent or superior laryngeal nerves, often from medical conditions or surgery. The left cord is more commonly affected due to nerve anatomy.
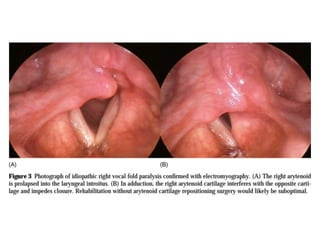
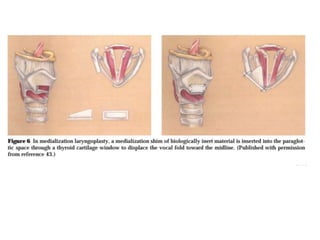
- Diagnosis involves laryngeal exam and sometimes electromyography or MRI. Treatment depends on severity but may include observation, vocal cord injections, framework surgery like medialization thyroplasty, or reinnervation surgery.
- Bilateral paralysis can be life-








![Theories on vocal cord in vocal cords paralysis
1. Semons law
In all Progressive organic lesions ,abductor fibres
[phylogenetically newer] are more susceptible and
thus first to be paralysed
2. Wagner and Grossman law
Total paralysis of recurrent laryngeal nerve immobilises
vocal fold in paramedian position because of intact
cricothyroid muscle
- Combined paralysis of RLN and SLN causes folds to be
in intermediate position](https://image.slidesharecdn.com/vocalcordpara-wpsoffice-231224041144-dc2ae719/85/vocal-cord-paralysis-presentation-larynx-18-320.jpg)
![Symptoms
hoarseness
hypophonia.
Dysphagia with possible frank aspiration .
PHYSICAL EXAMINATION
-neck examination
-cranial nerve examination[To rule out jugular
foramen syndromes, after stroke and
after skull base surgeries ]
-Flexible nasolaryngoscopy -](https://image.slidesharecdn.com/vocalcordpara-wpsoffice-231224041144-dc2ae719/85/vocal-cord-paralysis-presentation-larynx-19-320.jpg)







![Reinnervation.
Using nearby nerves [both the ansa cervicalis and the
hypoglossal nerve]
reinnervation generally improves the bulk and
tone of vocal fold muscle but will not restore
physiologic motion
Reinnervation is ideally suited when the vocal fold is
known to be completely denervated.](https://image.slidesharecdn.com/vocalcordpara-wpsoffice-231224041144-dc2ae719/85/vocal-cord-paralysis-presentation-larynx-34-320.jpg)